Groin pain: risks and prevention
Groin strain is behind only fracture and joint reconstruction in terms of lost time from sport due to injury. Andrew Hamilton investigates at the risk factors for groin injury in sport and what the research says about injury prevention.
 Washington Capitals scores a goal past Vegas Golden Knights goaltender Marc-Andre Fleury, 2018 Stanley Cup Final. Credit: Harry How/Pool Photo via USA TODAY Sports
Washington Capitals scores a goal past Vegas Golden Knights goaltender Marc-Andre Fleury, 2018 Stanley Cup Final. Credit: Harry How/Pool Photo via USA TODAY Sports
Groin injuries and the pain they produce can be a frustrating problem for athletes, especially those whose sports involve sprinting and/or rapid accelerations and decelerations. The exact incidence of groin injury in most sports is unknown because athletes can often play through minor groin pain and the injury goes unreported. In addition, overlapping diagnoses can skew the incidence. However, studies in this area generally suggest that groin injury accounts for between 2-5% of all sports injury(1). Of these, the most prevalent groin injury in sport is the adductor strain, which for example in football players accounts for an incidence rate of around 10%-18% of groin strains(2).
Other studies have indicated that groin strain accounts for around 10% of all injuries in elite Swedish ice hockey players, while Molsa et al reported that groin strains accounted for 43% of all muscle strains in elite Finnish ice hockey players(3). Meanwhile, another study showed that the incidence of groin strains in a single National Hockey League (NHL) team was 3.2 strains per 1000 player-game exposures(4) and Emery et al reported that the incidence of adductor strains among 26 US National Hockey League teams in the NHL increased from 2003 to 2009, with the rate of injury greatest during the preseason(5).
Table 1: Frequent causes of groin pain in competitive athletics
| Acute onset | Muscle injury (strain, muscle fibre rupture, fascicle rupture etc) -avulsion and apophyseal injury -fracture |
| Gradual onset | Adductor inflammation, insertional tendinosis -osteitis pubis, symphysitis -weak groin, inguinal hernia -pathology of the hip joint (labral lesions) -femoroacetabular impingement (FAI) -snapping hip (coxa saltans) |
| Spinal column disorders | Disc prolapse with nerve root inflammation -blockage in the lumbar spine region -spondylolisthesis |
| Nerve entrapments | Ilioinguinal nerve entrapment syndrome |
| Pelvic dysfunction | Functional impairment of the pelvis -blockage of the iliosacral joints -pelvic torsion |
| Muscular | Imbalance in the muscle strings |
Injury diagnosis
The groin and hip region is made up of a number of different structures that interact (see figure 1). These include the pubic bones and symphysis, musculature, tendons, aponeuroses, ligaments, the inguinal canal, hip joint etc. Consequently athletes often report a pain or pain pattern that cannot be uniquely assigned to a single structure. In addition, there are a multitude of various nerves in the groin region responsible for providing sensation and which support movement. Any compression of these nerves (entrapment syndrome) can lead to significant stress-related pain(6).
In addition to a detailed clinical investigation, clinicians therefore require a good knowledge of the (complex) anatomy of the groin and pelvic region, and an understanding of the interaction of affected structures. Furthermore, image-based diagnostics are extremely useful for a definitive diagnosis with respect to the numerous differential diagnostic-related causes. Table 1 provides a summary of possible differential diagnoses in which a distinction can be made between extra-articular causes (for example muscle and tendon injuries) and intra-articular sources of pain (for example femoroacetabular impingement and labral lesions)(7-10). Despite the large number of possible differential diagnoses, muscular injuries of the adductors, the iliopsoas muscle and abdominal musculature are the most frequent causes of acute groin pain in sportsmen and women. For example, a 2009 study looked at groin strain in elite European footballers who were playing for 23 of the top UEFA teams(11). Out of the 628 cases of groin strain, 399 (63.5%) resulted from adductor injuries, while injury to the iliopsoas muscle accounted for 52 (8.2%) cases – a combined total of nearly 72% of the reported groin injuries. More generally, studies indicate that among most competitive athletes between the ages of 20 and 30, the myotendinous junction is the mostly like site for muscle tears(7,12).
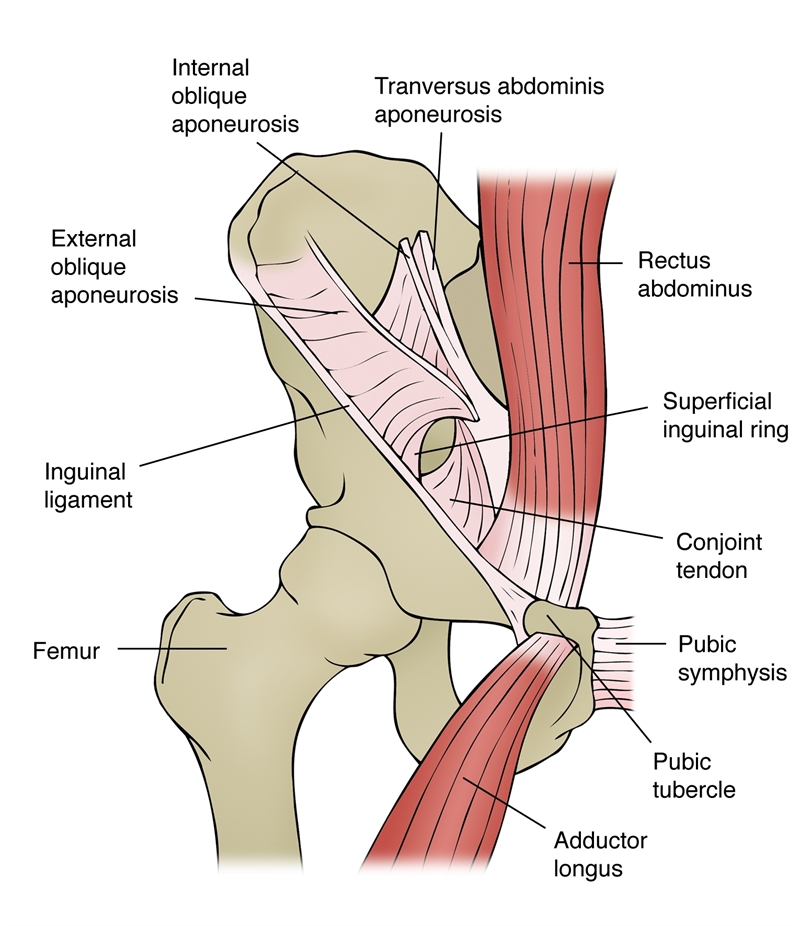
Figure 1: Simplified diagram of groin anatomy
Risk factors
On the basis that ‘an ounce of prevention is worth a pound of cure’, it’s pertinent to ask what are the risk factors that predispose an athlete to groin injury? In a 2013 paper, Bruckner et al. suggested that there are several factors that can predispose athletes to develop a groin injury(13). The researchers classified these factors as intrinsic and extrinsic (see box 1). It follows that appropriate conditioning programs addressing these factors can play an important part in groin injury prevention – or, indeed, a rehab program aim at speedy recovery and future prevention – something we’ll return to shortly.
There’s certainly solid evidence in the literature showing an association between strength or flexibility and musculoskeletal strains in various athletic populations. For example, in a study of footballers, researchers found decreased pre-season hip abduction range of motion in players who subsequently sustained groin strains, compared with uninjured players(14).
In professional ice hockey players, adductor muscle strength has been associated with subsequent muscle strain. For example, US researchers found that pre-season hip adduction strength was 18% lower in NHL players who subsequently sustained groin strains, compared with the uninjured players(4). The hip adduction:abduction strength ratio was also significantly different between the two groups; in the players who sustained a groin strain, the pre-season adduction: abduction strength ratio was lower on the side that subsequently sustained a groin strain (as compared with the uninjured side). Adduction strength was 86% of abduction strength on the uninjured side but only 70% of abduction strength on the injured side.
Another study on adductor strains in ice hockey players showed that players who practiced during the off-season were less likely to sustain a groin injury(15). In this study, an additional risk factor was the presence of a previous adductor strain – consistent with a study into Australian Rules football players, where researchers reported a 32% re-injury rate(16).
In a 2007 study, researchers conducted a systemic review of the literature for risk factors in groin injury(17). They concluded that there was support for an association of previous injury and greater abductor-to-adductor strength ratios as well as lack of sport specificity of training and pre-season sport-specific training, as individual risk factors in groin strain injury in athletes. They also stated that core muscle weakness or delayed onset of transversus abdominal muscle recruitment may increase the risk of groin strain injury. However, when it came to absolute levels of adductor strength and length, as well as age and/or sports experience, the evidence to support a causal association was only weak.
Coming right up to date, a systematic review published earlier this year evaluated the evidence for groin injury risk factors across a wide range of sports(18). The researchers identified 2521 potentially relevant studies, of which 29 were included and scored. The researchers concluded that the following factors are associated with groin injury: a previous groin injury, more elite levels of play, reduced hip adductor strength (absolute and relative to the hip abductors), and lower levels of sport-specific training.
Contributing factors in the development of groin pain
- Post-injury inadequate rehabilitation
- Muscle weakness
- Fatigue
- Inadequate muscle conditioning
- Decreased fitness
- Poor groin flexibility
- Muscle tightness
- Poor pelvic and core stability
- Inadequate warm up
- Increasing age
- Poor posture
- Neural tightness
- Recurrent injury
Prevention
In the introduction to this article, we looked at grain strain incidence. However, to focus purely on the incidence of this injury provides an incomplete picture of its impact because the morbidity attached to chronic groin pain means it is behind only fracture and joint reconstruction in terms of lost time from sport due to injury. That being the case, any strategies that can help prevent or reduce the risk of groin strain are invaluable.
In a recent review on sport-induced groin strain injuries, researchers proposed a number of extrinsic and intrinsic factors in the development of groin pain (see box 1)(19). It follows, therefore, that any prevention program should try to address one or more of these factors. Given that adductor injury accounts for a significant proportion of groin injuries overall, it’s pertinent to ask whether adductor strength training can help.
A study on strength training to prevent adductor strains in professional ice hockey players produced positive results(20). Before the 2000 and 2001 seasons, professional players were strength tested. Thirty-three of the 58 players were classified as at risk, with an adduction:abduction strength ratio of less than 0.8, and were placed on an intervention program consisting of strengthening and functional exercises aimed at increasing adductor strength. Injuries were tracked over the course of the two seasons and the results showed that injury incidence was 0.71 adductor strains per 1000 player-game exposures (approximately 2% of all injuries). This is compared with a pre-intervention injury rate of 3.2 per 1000 player-game exposures (approximately 8% of all injuries – 4 times higher). The validity of this intervention is supported by the fact that the pre-intervention injury rate in this study seems consistent with that in other studies on groin strain injury in ice hockey players(21).
In footballers, meanwhile, Junge et al. showed that a generalized conditioning program was suitable for injury prevention in young males of varied skill levels(22). The program was made up of ten exercises to improve endurance, reaction time, coordination, lower extremity stability, plus flexibility and strength of the trunk, hip, and lower extremities. In addition to nearly 50% fewer mild injuries, 41% fewer overuse injuries and 55% fewer training injuries, this program resulted in no less than 80% fewer groin injuries over the course of an entire year.
Further evidence for the benefits of strength training comes from a 1999 study on athletes(23). It found that 8-12 weeks of an active strengthening program proved effective in treating chronic groin strains. The program consisted of progressive resistive adduction and abduction exercises, balance training, abdominal strengthening, and skating movements on a slide board. This was in contrast to a passive physical therapy program of massage, stretching, which was ineffective.
An example of the kind of conditioning program that appears to help groin strain prevention in athletes who suffer recurring groin injuries is shown in table 2(24). The example given is for ice hockey players but can be adapted (in the sports-specific conditioning phase) for other sports too. This treatment regime combines different modalities: passive treatment immediately followed by an active training program, which emphasizes eccentric resistive exercises. Other studies provide solid evidence that this method of rehabilitation and prevention produces positive results(7,25).
Athletic pubalgia
Athletic pubalgia describes a condition where disruption and/or separation of the more medial common aponeurosis from the pubis occurs (usually with some degree of adductor tendon pathology), and is a common cause of chronic groin pain in athletes. Although most commonly observed in soccer and ice hockey players, athletic pubalgia can affect a wide variety of sportsmen from different age groups. However, despite several reports of athletic pubalgia in female athletes, it is almost exclusively found in men. The symptoms of athletic pubalgia are characterised by pain during sports movements”particularly, twisting and turning during single-limb stance. This pain usually radiates to the adductor muscle region and origin and to the testicles, and is often difficult for the patient to pinpoint. Following sports activity, the athlete may be stiff and sore, making practice and competition difficult. Indeed, any physical exertion that increases intra-abdominal pressure, such as coughing or sneezing, can cause pain. Athletic pubalgia occurs with weakening of the rectus abdominis, pyramidalis, internal and external obliques, transversus abdominis muscles, and/or the tendons in the region of the inguinal canal (where inguinal hernias occur “ see Figure 1). However, when an inguinal hernia occurs because of weakening of the abdominal wall, a hernia may be felt. By contrast, while there is weakening or tears in the abdominal wall muscles in athletic pubalgia, there is no palpable hernia. Indeed, physical examination findings are subtle, and most tests do not definitively confirm the diagnosis. Unlike most groin strain injuries, athletic pubalgia does not respond to strength and conditioning rehab programmes or other therapies. In fact, the evidence suggests that all non-operative treatments of athletic pubalgia will fail to provide a resolution of symptoms. By contrast, surgical intervention almost always results in a pain-free return to full activity.
The role of warm ups
One element of groin strain prevention that may also be important is an appropriate warm-up. Although there’s a dearth of groin-injury-specific studies into warm-up, a 2004 study on 315 adult male professional footballers in US Major League Soccer provides valuable insight(24). In an effort to reduce the rate of groin injury, a comprehensive 20-minute warm-up program was developed as an alternative to a conventional warm-up program.
This 20-minute warm-up program was used 2-3 times per week during the 2004 season. The players were enrolled into one of two groups:
- Group 1 – 106 participants who performed the specially developed groin injury prevention warm-up before training and playing;
- Group 2 – 209 participants who served as the matched control group (age, sex, skill) and who continued with their usual warm-up routines
The program itself consisted of a combination of dynamic stretching, core strengthening, and pelvic proprioceptive exercises to encourage a neutral pelvis during dynamic activities using the lumbar paraspinals, multifidus, rectus abdominus, transversus, internal and external obliques, abductors, adductors, and hip external and internal rotators.
The results showed that the overall incidence of groin injuries occurring over the course of the subsequent season in the intervention group was 0.44 injuries per 1000 hours of sport practiced. This compared with a rate of 0.61 injuries per 1000 hours in the control group – ie, a reduction of 28%. The incidence of athletes requiring groin surgery in the intervention group was also lower at 0.13 per 1000 hours, compared with the control group’s incidence of 0.18 per 1000 hours – likewise, a reduction of 28%.
Table 2: Example of adductor strain injury prevention program (ice hockey)
| Warm-up | Bike |
| Adductor stretching | |
| Sumo squats | |
| Side lunges | |
| Kneeling pelvic tilts | |
| Strengthening program | Ball squeezes (legs bent to legs straight) |
| Different ball sizes | |
| Concentric adduction with weight against gravity | |
| Adduction in standing on cable column or elastic resistance | |
| Seated adduction machine | |
| Standing with the involved foot on a sliding board moving in a sagittal plane | |
| Bilateral adduction on a sliding board moving in the frontal plane (i.e., simultaneous bilateral adduction) | |
| Unilateral lunges with reciprocal arm movements | |
| Sports-specific training | On ice kneeling adductor pull togethers |
| Standing resisted stride lengths on cable column to simulate skating | |
| Slide skating | |
| Cable column crossover pulls | |
| Clinical goal Adduction strength at least 80% of the abduction strength |
Summary and conclusions
Groin injuries in athletes span a wide range of conditions and are a major cause of missed time from sports. To make matters worse, once a groin injury has occurred, an athlete is at increased risk of a future groin injury. The good news is that many common groin injuries (e.g., involving the adductor muscles) respond well to strength and conditioning programs – both as part of a post-injury rehab program and in terms of prevention. These programs should aim to provide passive treatment, immediately followed by an active training program emphasizing eccentric resistive exercises. The evidence also suggests that warming up using a combination of dynamic stretching, core strengthening, and pelvic proprioceptive exercises can significantly reduce the risk of injury in athletes – even those with no previous history of groin injury.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










