Knee microfracture- Part II: post-surgical rehabilitation
In part one of this 2-part series, Chris Mallac looked at chondral and osteochondral injuries to the patellofemoral joint, outlining the important pathophysiology and characteristic mechanisms for this injury and presenting signs and symptoms when this injury occurs. In part two, he considers the postsurgical rehabilitation of microfracture procedures.

Chondral and osteochondral defects of the patella and/or trochlear groove can be debilitating injuries for the athlete that often will need surgical intervention. The rehabilitation following surgery can be lengthy and involved, with a firm commitment from the patient to ‘buy in’ to post-surgical rehabilitation.
A significant amount of work on microfracture techniques and the subsequent rehabilitation postoperatively has been provided by Dr J Richard Steadman(1-4). Many of the ideas provided in this section are drawn from suggestions by the above author and also Tyler and Young(5).
It is difficult to prescribe an exact time-dependent or criteria-dependent rehabilitation protocol for microfracture procedures as the healing time is directly influenced by the size of the defect and also the body weight of the patient. Big lesions (>400mm2) in heavier athletes will take much longer to recover than smaller lesions (200mm2) in lighter athletes. The progression through stages is dependent on these two factors as well as the reaction of the post-surgical knee to increases in loading. If the knee reacts with pain and/or effusion post-loading, then the load is too great and needs to be reduced for the next session.
What is consistent in rehabilitation is the purpose of the initial phase of recovery, where it is important to provide an optimal physical environment via protected weight bearing and passive movement to allow the mesenchymal stem cells that leak into the surgically created marrow clot to differentiate and produce new cells and an extracellular matrix. With time these cells and matrix will mature to form durable repair tissue in the original defect. Any early loading on this tissue has the capacity to damage the healing tissue and result in a failed repair; therefore, loaded movement is restricted in the early postoperative period and gradually reintroduced to allow adaptation in the newly formed fibrocartilage to occur(1). Studies on primates with microfracture procedures showed that at six weeks postoperation, the repaired cartilage showed limited repair of chondral tissue, but at 12 weeks, the bone showed improved repair with a more mature hyaline cartilage(6). These findings suggest that restrictions in weight-bearing and protection of the defect site may be warranted for greater than six weeks to allow the tissue repair to adapt to increased stress.
Continuous Passive Motion
After surgery, all patients are placed in a continuous passive motion (CPM) machine to encourage a range of movement and to encourage tissue maturation for the first three months following surgery (see figure 1). The use of CPM after microfracture has demonstrated improvements in cartilage lesion grades in patients with full-thickness chondral defects (see box 1)(7).
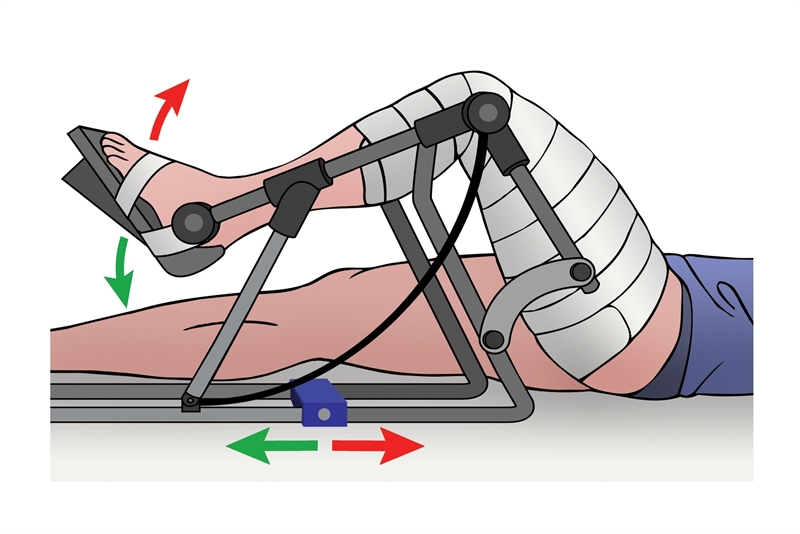
Figure 1: CPM machine
Passive motion exercise, with and without CPM
For injuries to the tibia or femur, the CPM machine is set to 30° to 70° at a rate of one cycle per minute for eight hours per day, and for injuries to the patellofemoral joint the CPM is limited to 0°-50° to prevent the prevent the patella engaging in the trochlear groove. Patients who cannot access CPM machines are encouraged to perform 500 flexion/extension ROM exercises three times per day. The following exercises can also be performed for patients without a CPM: Extension -Passive extension — sit in a chair and place your heel on the edge of a stool or chair; relax thigh muscles and let the knee sag under its own weight until maximum extension is achieved. -Heel props — place rolled up towel under the heel and allow leg to relax -Prone hangs — lie face down on a table/bed with the legs hanging off the edge of the table; allow the legs to sag into full extension. Flexion-Passive flexion — sit on chair/edge of bed and let knee bend under gravity (you may use the other leg to support and control flexion). -Wall slides — Lie on your back with the involved foot on the wall and allow the foot to slide down the wall by bending the knee; use other leg to apply pressure downward. -Heel slides — Use your good leg to pull the involved heel toward the buttocks, flexing the knee. Hold for five seconds; straighten the leg by sliding the heel downward and hold for five seconds.
Weight-bearing
The patient is instructed to only ‘touchdown weight bear’ for the eight weeks following surgery to avoid any muscle contraction around the knee that may lead to compression of the tibiofemoral joint and/or patellofemoral joint. For injuries to the tibiofemoral joint, a motion-limiting brace is not worn, but for a patellofemoral lesion, the knee a brace is suggested and is braced at 0°-20° extension to avoid any flexion of the knee, which may result in the patella contacting the femoral trochlear groove and create shearing at the maturing marrow clot. The brace is to be worn at all times except when the patient is in the CPM machine.
Given that the femoral condyles are weight-bearing surfaces, restrictions are placed upon the amount of weight a patient is allowed to place upon the involved lower extremity. However, patellofemoral lesions are able to take more weight initially (up to 30% body weight), and then this is progressed to weight bearing as tolerated in the brace from two weeks post-operation. For larger lesions of the patellofemoral joint (>400 mm2), weight-bearing is protected for the first six weeks.
After the initial eight weeks, the patient can increase the weight-bearing as tolerated. The patient with a patellofemoral lesion is encouraged to fully weight bear in the knee motion brace from eight weeks onwards. However, the brace is gradually opened to allow more knee flexion. Patients are gradually weaned off crutches over weeks nine and ten, and the brace is removed at ten weeks post-operation.
Passive physiological and accessory manual therapy
In tibiofemoral lesions, patellar mobilizations and patella/quadriceps mobilizations are commenced immediately to prevent adhesion forming between the patella and femur. This is also encouraged in patellofemoral lesions. Full passive range of motion movements into flexion and extension are encouraged from early post-operative stages, except for the patellofemoral lesions, where flexion is not encouraged. Manual therapy is a defining feature in the first 12 weeks after surgery. Once the full passive range of motion is restored with full extension and full flexion (and no ongoing knee effusion), the emphasis moves away from the range of movement and progresses to strengthening.
Strengthening
Gentle non-weight bearing quadriceps contractions are encouraged from an early stage, such as inner range quadriceps setting, straight leg raise, and muscle stimulators (on the atrophy setting), and this is continued for the first 12 weeks after surgery. At this stage, supine/side lie/ prone hip exercises are encouraged with resistance to maintain some proximal hip muscle hypertrophy.
At 12 weeks post-surgery, the patient should have close to the full range of passive and active movement, and strength training can be safely progressed. In tibiofemoral lesions, the ranges of motion allowed for strengthening are initially limited to 0 degrees to 300 degrees during this 12+ week stage of rehabilitation. Full weight bearing is allowed as the patient feels comfortable; however, the range is always limited in this period.
In patellofemoral lesions, the surgeon will note during surgery at which point of knee flexion the patella enters the trochlear groove and moves over the newly created marrow clot. For example, in a small patella lesion, the surgeon may note that the patella contacts the femur from 20-40° of knee flexion, but before and after this range, there is no patella-to-femur contact. Loading the knee joint in flexion is then avoided in this 20-40° range for the first four months postoperation but loading up to 20° and from 40° onwards is permitted.
Loading may take the form of single-leg squats, one-legged leg presses, and Bulgarian split squats (see figure 2). These are the exercises that are easiest to control in terms of speed, tempo, and range of movement. Isometric holds can be added at the maximum knee flexion angles, and muscle stimulators can also be used in conjunction with these movements.
The focus of the 12-16 weeks post-surgery is to build some quadriceps and hamstring endurance in safe positions prior to the strength emphasis in weeks 17 onwards. Exercises can gradually progress from weeks 17 to 24 to incorporate pain-free ranges of knee flexion and a gradual increase in load. More sports-specific lifting, such as Olympic weight lifting, is delayed until simple single-leg movements can be performed through range and without pain. It may be necessary at this stage to still protect larger lesions from the painful range of movement.
Hip-dominant movements that do not involve knee flexion under load can also be progressed at this stage. Exercises such as single-leg Romanian deadlifts, hip/ hamstring bridge with the knee at safe flexion angles, back hyperextension and reverse hyperextensions are all safe to load and increase at this stage. From week 24 onwards, it is expected that the patient will now be comfortable enough and have sufficient strength to progress to more traditional strength training programs, incorporate more explosive Olympic lifts and start easy plyometrics-type movements. These are all gradually increased through the final stages of rehabilitation.
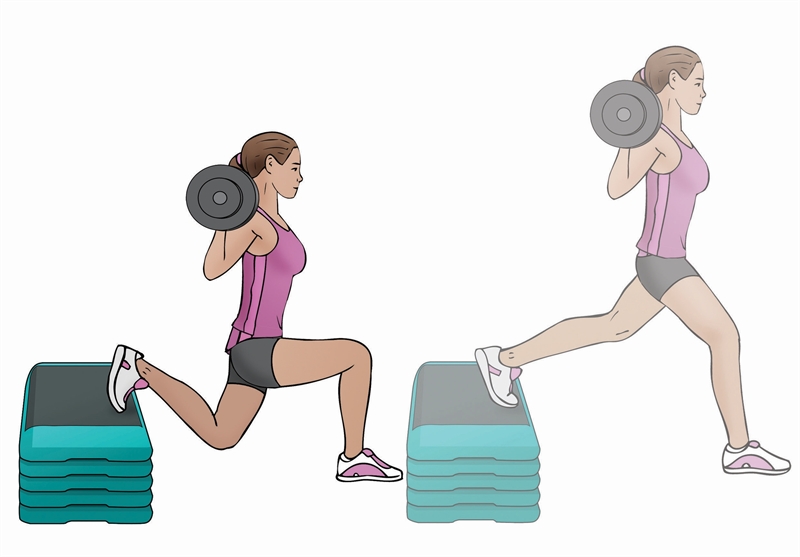
Figure 2: Bulgarian split squat
Cardiovascular training
In tibiofemoral lesions, gentle spinning on the bike and deep water running (no touching the pool bottom) can be started as soon as one-week post-operation if the lesion is small. However, in larger lesions (>400mm2), this is delayed to 4 weeks post-surgery. At 12 weeks post-surgery, most non-impact cardio work is allowed, such as spinning, water running, elliptical, and treadmill walking.
Spinning on the bike is done initially without resistance until the patient can achieve a comfortable 45 minutes pain-free and without post-exercise effusion. Then the load is gradually added and the time is reduced to 20 minutes. This is built up again to 45 minutes before another increase in load is allowed. Treadmill walking is encouraged at a 7° incline initially at 12 weeks post-op and limited to 10 minutes. This is gradually increased 5 minutes per session, assuming the knee suffers no pain and no post-exercise effusion.
Simple running mechanics drills can be started at 16 weeks post-operation, with an emphasis on drills to improve hip/ knee/ankle mobility. Actual running can be performed on a soft surface such as grass or a treadmill, with only short running intervals (1 minute) interspersed with longer walking intervals (4 minutes). The running time is increased by one minute each week, and walking time is reduced each week so that after five weeks, the patient should be able to run 20 minutes continuously.
If specific load-removing devices are available such as Alta G treadmills, then the program is modified to allow continuous running for 20 minutes, but at 50% body weight. Bodyweight is increased by 10% each week so that by five weeks, they are up to 100% body weight. Speed and agility drills are actively commenced at around 21 weeks post-operation and gradually increased over a 4-5 week period.
By 26 weeks post-operation, the athlete should now be able to perform most of the mobility, speed, and agility-type drills prior to being reintegrated back into team training. Generally, athletes in high-impact sports that involve landing, cutting, pivoting, and sudden deceleration may take nine months to fully recover their physical abilities and also the confidence needed prior to returning to competition.
Long-term impairment
The long-term outcomes following a microfracture procedure demonstrate that some impairment to athletic function can be expected. When the microfracture procedure was performed in a group of athletes, improvements in function were initially seen. Lysholm’s knee scores improved from 56.8 to 87.2 after surgery, while Tegner’s scores rose from 3.2 to 6 at the two-year follow-up. The athletic population showed an 80% improvement in sports activities during the initial two years, but this gradually declined to 55% at five years. This can be attributed this decrease to the natural decline in one’s ability to perform at a high level with age as well as the possibility that the fibrocartilaginous repair tissue has less resilience and may deteriorate over time(8).
However, those athletes who have undergone a microfracture procedure will have the expectation that they will be back in competition in a timeframe of 6-9 months following surgery. Once they have progressed through the stages of rehabilitation, particular outcome measures can be used to determine the key exit criteria for a full return to sport. These are:
- Minimal knee effusion post training
- Full active loaded knee flexion (single leg squat)
- Return to maximum running velocities
- Confidence in landing and changing direction
Conclusion
Knee micro-fracture procedures involve a lengthy rehabilitation process that involves controlled passive movement with protected weight bearing. Due to the debilitating effects of prolonged non-weight-bearing and lack of aggressive quadriceps exercises in the early postoperative period, the patient can expect significant quadriceps wasting and functional limitation at the ten to twelve-week point following surgery. Therefore regaining a full range of movement and redeveloping quadriceps muscle strength will take a long protracted rehabilitation period. When the athlete has gained sufficient weight-bearing strength, then returning to functional capacities such as running and changing direction will also be a lengthy time-dependent endeavor. Patience and consistency are required by both therapist and patient to slowly regain function, with an expected time to return to sport confidently often being greater than nine months in duration.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










