Levator Scapulae: Why Length Matters
Chris Mallac discusses the relevant anatomy and biomechanics of the levator scapulae muscle, how it is implicated in dysfunction around the shoulder and cervical spine, and also rehabilitation strategies to stretch and loosen this muscle

The Levator Scapulae (Lev Scap) is a muscle that has often been implicated in pain and dysfunction in the upper quadrant. It may create pain and dysfunction in and around the shoulder but it can also create pain and dysfunction in the cervical spine and may lead to cervicogenic headaches. It is often a muscle that becomes chronically tight, shortened and overactive, exerting its effect on both scapula position and cervical spine movements.
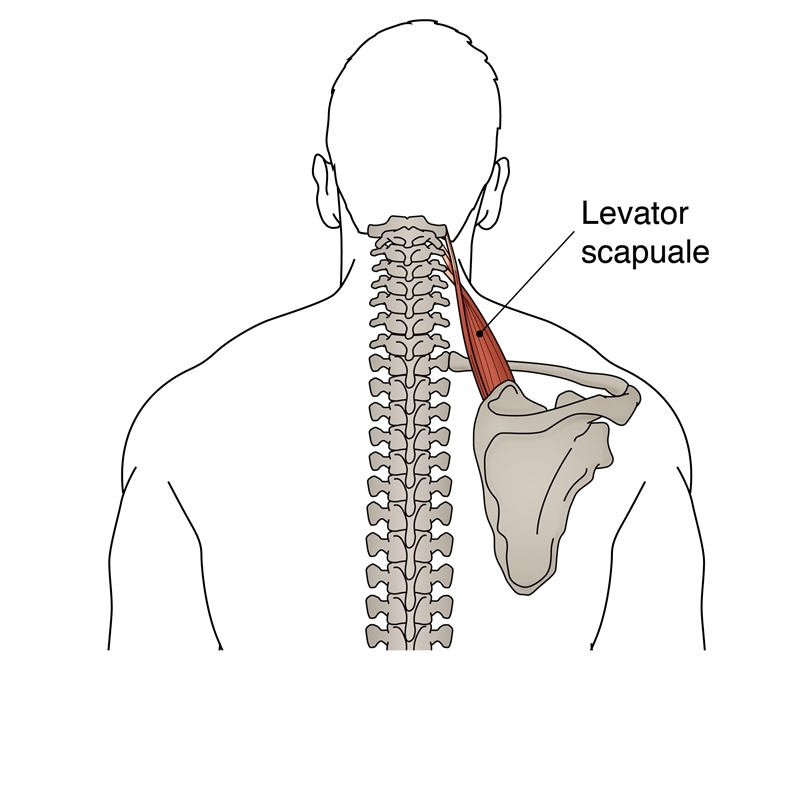
Figure 1: Levator scapulae anatomy
Anatomy and biomechanics
The Lev Scap originates on the cervical spine from the posterior tubercles of the transverse processes of cervical vertebrae 1-4 (see figure 1). It courses downwards and laterally to insert onto the medial border of the scapula at the level of the scapular spine. The Lev Scap may lie deep to the sternocleidomastoid at its origin, deep to the splenius capitis at its mid-portion, and deep to the trapezius at its lower portion. As the muscle descends it twists 180 degrees so that the most superior fibres insert medially and the lowermost fibres insert more laterally(1).
In a study on 30 cadavers, Menachem et al (1985) found that in 63% of cadavers, the Lev Scap was inserted on the scapula in two layers enfolding the medial border of the scapula(2). Some of the scapular attachment was on the underside of the scapula and not readily palpable. In nearly half of the cadavers, a bursa was found in the areolar tissue between the two layers, and in 43%, a narrow band of the serratus anterior was reflected over the medial border of the scapula around its upper angle, close to the attachment of the Lev Scap.
In 5 of these 13 (38%) another bursa occurred between the serratus anterior, the angle of the scapula, and the Lev Scap. This study suggests that this syndrome, leading to bursitis and pain, may be caused by anatomic variations of the insertion of the Lev Scap and origin of the serratus anterior. This may explain the constant trigger point and crepitation as well as the increased heat emission found on thermography. It may also explain why local steroid injections relieve symptoms partially in 75% of those patients who undergo treatment(2).
Innervation is provided by the cervical plexus (C3, C4), with the nerves passing posterior to the sternocleidomastoid muscle and coursing downwards to the posterior triangle of the neck – thus innervating the Lev Scap. It also has frequent contributions from the dorsal scapular nerve(3).
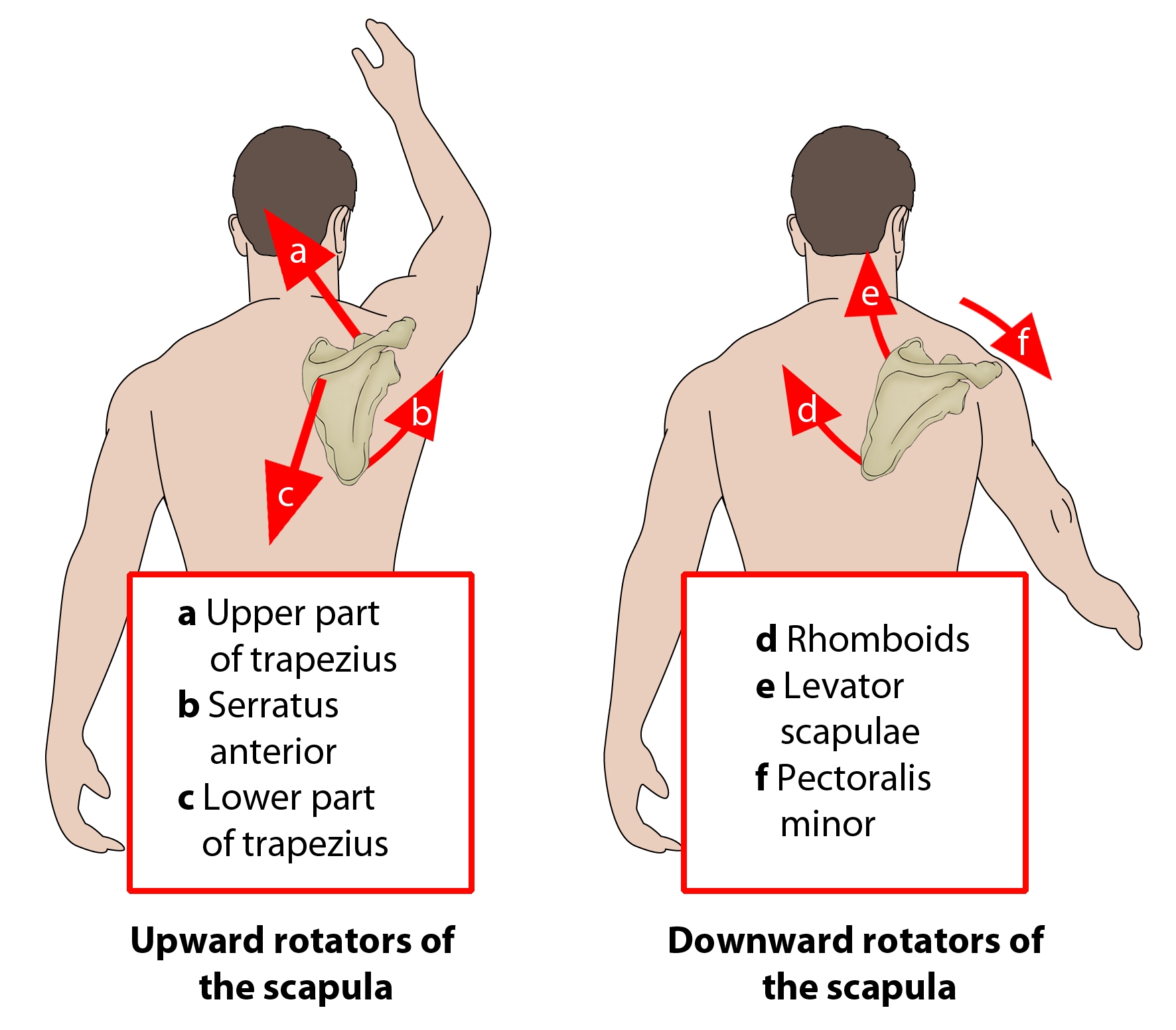
Figure 2: Function of levator scapulae
Function
With the cervical spine fixed, the Lev Scap functions to elevate the scapula and to tilt the glenoid cavity inferiorly by rotating the scapula downward (see figure 2). It couples with the pectoralis minor and rhomboid as a downward rotation muscle. Furthermore with the scapula fixed and acting unilaterally, the Lev Scap can laterally flex and rotate the vertebrae ipsilaterally. If acting bilaterally, it can assist in cervical extension(1,4).
In EMG studies of Lev Scap, DeFreitas et at (1979, 1980) found in that it was strongly active in abduction and elevation, moderately active in shoulder flexion and minimally active in scapular retraction and shoulder extension(5,6). DeLauter (1982) added that Lev Scap contracts concentrically during the first half of abduction and eccentrically during the second half of abduction(7). Due to greater force production during an eccentric contraction, this indicates that the force exerted by Lev Scap is greatest during the second half of abduction range.
It is interesting that the Lev Scap is active during shoulder elevation, and that it works eccentrically during the later stage of abduction. This would seem counterintuitive as it would prevent upward rotation of the scapular if it contracted during shoulder abduction. The possible mechanism to explain this may be that it is attempting to prevent the depressing effect of lower trapezius that also contracts strongly during the later stages of upward rotation(8). This allows the upper trapezius to exert its maximum effect in late stage abduction to assist with upward rotation of the scapula as well as elevating the scapular to allow the acromian process to be cleared away from the humeral head in order to avoid a subacromial impingement(8).
During postural tasks the Lev Scap also acts to elevate the scapula along with the upper trapezius and upper serratus anterior, and it also works isometrically to support the scapula in the event of a traction type effect on the shoulder girdle such as carrying a shoulder bag or shopping bags in the hand(1).
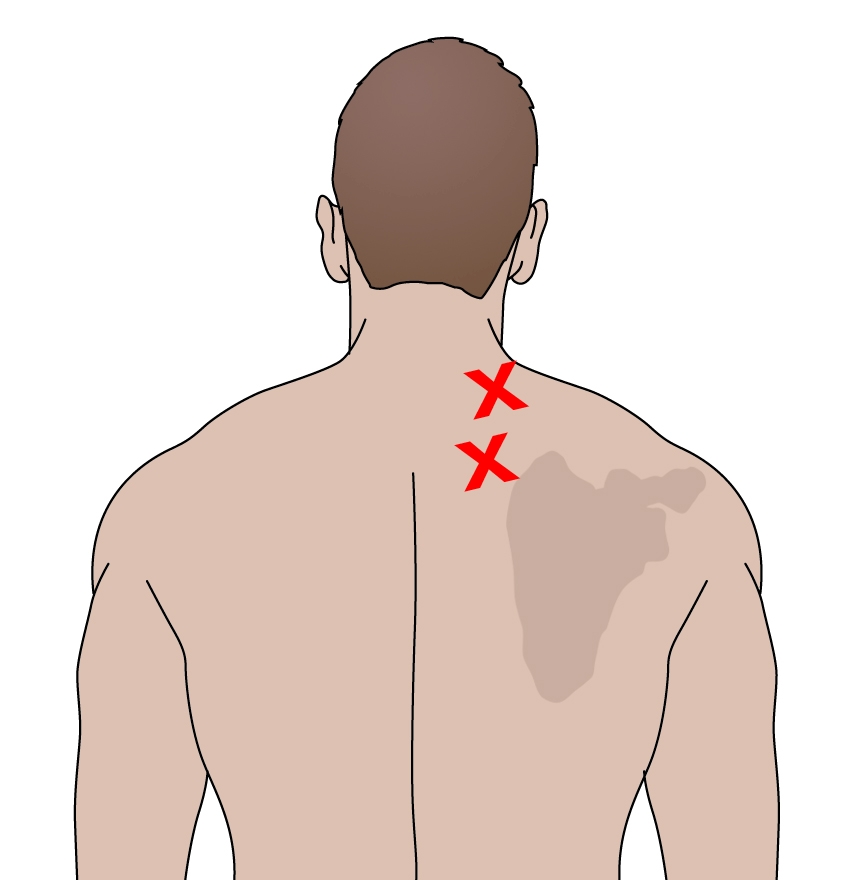
Figure 3: Myofascial trigger point location and referral pattern
Role in dysfunction
Myofascial trigger points (figure 3) are a common finding in the Lev Scap muscle. It has been found that in normal healthy subjects, about 20% have latent trigger points in this muscle, and it is the most common muscle to suffer from active trigger points(9,10). When active, these trigger points will create a ‘stiff neck syndrome’ and rotation towards the same side will be painful due to muscle contraction. Rotation away will also be painful due to a stretch imposed on the muscle. The referral pattern of Lev Scap trigger points has been well described previously by Travel and Simons (1999)(1).
Potentially hazardous positions and occupations that may activate trigger points in the Lev Scap include:
- Sustained head/neck rotation at work (secretarial work).
- Carrying a bag or purse on the shoulder for an extended period.
- Sleeping with the muscle in a shortened position or in an airline seat.
- Constant extension of the neck to look upwards (screen or stage).
- Repeat rotation – ‘spectator neck’.
- Vigorous athletic movements that need scapula movement as well as cervical movement. For example, looking up whilst performing a chin up movement.
Dr Vladimir Janda has suggested that shoulder pathologies such as subacromial impingement could result from a characteristic pattern of muscle imbalance including weakness of the lower and middle trapezius, serratus anterior, infraspinatus, and deltoid, coupled with tightness of the upper trapezius, pectorals and Lev Scap(11). This pattern is often referred to as part of Janda’s ‘Upper Crossed Syndrome’.
Lev Scap may also cause more direct cervical spine pathology, as the Lev Scap insertion acts through the upper cervical facet joints. As Lev Scap exerts an increasing amount of force on the cervical spine during outer range shoulder abduction, an increase in loading on the cervical joints must occur. Due to the action of Lev Scap on the cervical spine, it may create compressive loading on the facet joints and to also hold the cervical spine slightly into laterally flexion and rotation of the spine ipsilaterally(12).
However, often there is minimal movement of the cervical spine indicating that synergistic muscle action is occurring to isolate Lev Scap action to the scapulothoracic joint. The results at the cervical spine may be then an increase in compressive loading which will result in increased intradiscal pressure and increased facet joint compaction. Mechanically both the facet joint and disc will become distorted and compressed. This distortion may produce a pain response, including the production of referred pain which may be experienced in the shoulder.
Assessment
A thorough examination will entail a full history of possible precipitating factors. It may become apparent in the questioning that some manner of athletic or work stress that has overworked and contracted the Lev Scap may be present, such as repetitive overhead activity or strong traction type forces on the muscle from weight lifting or postural stress. Usually the pain and discomfort in the neck will build over a number of days due to repetitive overuse. Commonly the definitive clinical feature associated with Lev Scap tightness is an inability or unwillingness to move the head/neck into rotation. Usually flexion and extension are pain-free. Only in chronic cases of Lev Scap tightness will full shoulder abduction be limited. However, the patient may present with shoulder pain and pathology that is associated with Lev Scap overactivity, as the scapula will become positioned into downward rotation with the medial supero-medial border in elevation.
The two primary areas where trigger points can be palpated are 1) along the angle of the neck where the muscle emerges from under the anterior border of the upper trapezius and 2) a tight band that can (usually) be felt on the supero-medial scapula border where the muscle has an enthesis on the scapula.
Treatment
Managing chronic tightness and overactivity in the Lev Scap is best addressed in rehabilitation with stretching and selfmassage for underlying trigger points. More aggressive interventions include direct trigger point injections into the chronic trigger points present in the Lev Scap. For the purposes of this article, only self-stretches and massage techniques will be discussed.
Summary
The Lev Scap works with other scapular downward rotators to control scapula posture. It often becomes tight and overactive, along with other downward rotators such as the pectoralis minor. This may then create scapula dyskinesis that may lead to shoulder pathology such as impingement syndromes and rotator cuff damage. Furthermore, due to its attachment on the upper cervical facet joints, it may lead to cervical pathology and headaches related to the neck.
As it is often a muscle that becomes chronically shortened and overactive, it is a muscle that rarely needs strengthening. More often, it is a muscle that responds to stretch and trigger point therapy. This article has presented two common techniques to both stretch the muscle and reduce inherent trigger points in the muscle.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









