Long head of biceps tendon - Part II : the road to recovery

Athletes involved in sports that require a lot of overhead hand/arm position are vulnerable to long head of biceps tendon (LHBT) pain due to the possible compressive and tensile forces encountered by the tendon within the surrounding bones and soft tissues (as discussed in part one). Therefore, this condition is quite common in swimmers, cross fit athletes, tennis players, gymnasts and Olympic weightlifters just to name a few. Furthermore, the LHBT may also be injured due to strong contractile forces applied by the attached biceps muscle. This would be more common in athletes such as rugby players who are making tackles and throwers such as baseball pitchers.
The main subjective symptoms experienced by those suffering from LHBT pain are as follows:
- Pain is located primarily at the anterior part of the shoulder, often at the bicipital groove, or deep under the acromian process. The cross over of symptoms with subacromial bursitis, rotator cuff pathology and frank labral pathology is very common and often difficult to separate clinically.
- Pain at rest, night pain and pain on rotation are common especially in the event of a tenosynovitis with an inflammatory component.
- The pain may also radiate down the arm and muscle belly, sometimes reaching the radial aspect of the hand, but this usually lacks a precise distribution. It may also co-exist with paraesthesia in this distribution. This would be a differential for a suspected C6 radiculopathy. This is different to the classic ‘deltoid area’ pain suffered by those with supraspinatus pathology.
- A clunk or click may be felt along the bicipital groove with an unstable and subluxing LHBT.
- While the clunk of a subluxing and unstable biceps tendon is classic when the shoulder is rotated (especially in abduction) this clinical sign is uncommon in true dislocations of the LHBT as dislocations are usually irreducible.
| The typical objective clinical signs of LHBT pathology are as follows: |
|---|
| • Palpation of the tendon in the groove is usually painful and is best performed with the arm in 10Ëš of internal rotation(1). |
| • In dislocations of the LHBT, the tenderness is more medial on the lesser tuberosity, and the tendon can sometimes be rolled under the ï¬ngers. |
| • Several provocative tests have been described for isolating pathology of the LHBT, but the speciï¬city of these provocative tests is somewhat limited(2-4). These include Yergason’s test and Speed’s test. |
| • The 3-pack test has been described for assessing LHBT pathology(4). This test has excellent inter-rater reliability, sensitivity, and negative predictive value, and is a critical screening tool for LHBT injuries. Hidden extra-articular bicipital tunnel disease can reliably be excluded based on negative tenderness to palpation or a negative O'Brien sign. The 3-pack test consists of:o Active compression test(5) (O’Brien’s test — see figure 1 below)o Resisted throwing testo Biciptal tunnel palpation |
| • In the event of a LHBT dislocation, the patient presents with a loss of active elevation above 90Ëš, and it is common to ï¬nd a limitation of active and passive external rotation because the dislocated biceps tendon restrains the inferior part of the subscapularis. |
| • The ‘hourglass’ bicep sign can be evaluated by observing active and passive elevation of the arm. There is usually a limitation of the terminal 10Ëš to 20Ëš of active and passive elevation. This corresponds to a true mechanical locking of the shoulder, although there is no loss of rotation. However, this should not be confused with a frozen shoulder(6). |
| Pain provoking position of adduction and internal rotation |
|---|
 |
| • Have the patient standing with forward flexion, the arm to 90 degrees with the elbow in full extension.• Adduct the arm 10 degrees to 15 degrees medial to the sagittal plane of the body.• Internally rotate the arm so that the thumb points downward.• The examiner stands behind the patient and applies a uniform downward force to the arm. Pain will usually be felt deep in the shoulder.• With the arm in the same position, fully supinate the palm and repeat the manoeuvre.• The test is considered positive if pain was elicited during the first manoeuvre and is reduced or eliminated with the second. |
Imaging
*Plain radiographyPlain X-rays have only a limited ability in diagnosing abnormalities of the LHBT. They may be used to view the presence of calcification in the bicipital groove and bony deformity caused by fracture or osteophytes. What may also be seen are cystic changes in the lesser tuberosity, which may be a sign of tendinosis, or a tear of the upper subscapularis tendon (associated with lesions of the pulley system). Useful views are the anteroposterior in external rotation, the axillary and a modified axial (the Fisk view), which can demonstrate the anatomy of the groove(7,8).
*Ultrasound
Ultrasound allows a dynamic evaluation of the LHBT, the rotator cuff and the subacromial bursa in the differential diagnosis of anterior should pain. Ultrasound has excellent sensitivity and specificity in the diagnosis of subluxation and dislocation of the LHBT, and for visualising ruptures of the LHBT(9). However, it is not reliable for the detection of intra-articular partial thickness tears.
*MRI
Although this is the most widely used investigation in detecting LHBT lesions, the agreement between MRI and arthroscopic findings has been shown to be poor(10). The use of MR arthrography is preferable for detecting lesions of the biceps or of the pulley system, and is the investigation of choice for SLAP lesions.
*Arthroscopy
Arthroscopy is the gold-standard technique for the diagnosis of lesions of the LHBT. It allows a definitive diagnosis to be made(11). A dynamic examination of the tendon can be made by examining the movement of the LHBT within the shoulder by physically drawing the tendon into the joint. Furthermore, the shoulder can be elevated and rotated with the elbow in extension to visualise the ‘hourglass’ tendon(6)or signs of instability(12). The subscapularis can be viewed for hidden lesions not seen on MRI.
Conservative management
The conservative management of LHBT lesions will be limited to the spectrum of injuries that relate to tendinopathy and tenosynovitis. These will respond to the treatment paradigm aimed at reducing pain and improving function, which is paramount in the management of tendinopathy. These will be discussed below.Injections of cortico-steroid and local anaesthetic in and around the bicipital groove and sheath may have both a diagnostic and a therapeutic role. Intra-articular injections can relieve bicipital symptoms, but they may be ineffective if adhesions or synovitis restrict the dispersal of the injection into the bicipital groove. Such injections have been reported to be associated with tendon rupture(13).
Physiotherapy interventions
In the event of a chronic tendinopathy of the LHBT, the usual factors the physiotherapist needs to consider in the conservative management of this condition are the following:- Relative rest- The athlete needs to avoid the provoking activities that increase the pain in the tendon, being particularly mindful of overhead positions in sports. This may require a good four to six weeks avoiding compressive positions to allow time for the activated tendon tissue to settle and become less painful.
- Early isometrics- The paradigm of treatment for an irritated tendon in the reactive stage is to perform high load isometric exercises in positions that do not compress the tendon(14). For the LHBT, this may be performing resisted isometric elbow flexion and forearm supination in positions of neutral shoulder flexion/extension (arm by side). Positions that compress the tendon such as full extension backwards, full overhead positions will need to be initially avoided. The usual program is five sets of 45-second holds with a long rest between efforts. The effort needs to be high enough to induce some strong contraction in the bicep without an increase in pain above a 3/10 level on the visual analogue scale.
- PNF strengthening- As the tendon settles with pain, the LHBT tendon can be strengthened using PNF patterns such as the D1 and D2 flexion patterns, which maximise the use of the biceps muscle (see figures 2 and 3 below).
- Correct the associated pathomechanics- In and around the scapula and glenohumeral joint, such as weak serratus anterior and upper trapezius in the overhead athlete, and tight pectoralis minor and major and latissimus dorsi. The rotator cuff may need to be strengthened in the event of cuff weakness that causes a compensatory increase in LHBT involvement to stabilise the humeral head. Direct subscapularis activation exercise can also be used to strengthen the ‘biceps pulley system’.
- Gradual re-introduction of load - exposes the tendon to higher compressive and tensile forces to allow adaptation of the tendon.
Figure 2: PNF D1

Left = Start position; Right = Finish position
Figure 3: PNF D2
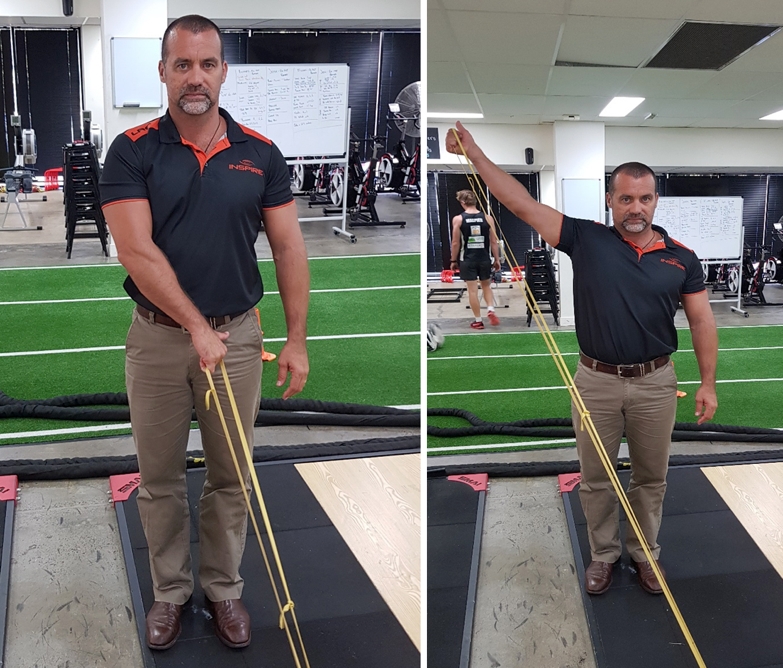
Left = Start position; Right = Finish position
Surgical treatment
Many conditions of the LHBT, such as frank instability of the tendon and dislocation, are more often cases that require surgical intervention. It is beyond the scope of this article to discuss the myriad of options for surgery that relate to disorders of the LHBT and how they differ. Therefore, the discussion will be limited to simply explaining the variations in surgical options available for LHBT lesions. The operative treatment for LHBT disorders will depend on factors such as age, level of activity, sports participation, occupation and type of injury.*Synovectomy and tendon debridement
Debridement is an option for patients with superficial fraying of the tendon without associated disorders in the shoulder such as rotator cuff tear and/or labral pathology. Debridement of the intra-articular portion of the tendon has been proposed in partial tears or with delamination involving less than 25% of the tendon(15). Arthroscopic synovectomy of the tendon sheath in the groove can relieve symptoms, and is probably applicable only when a mild amount of inflammation of an otherwise intact tendon is present(16,17).
*Biceps relocation and reconstruction of the pulley
Reconstruction of the damaged pulley (including subscapularis and supraspinatus) was proposed by some authors for the treatment of biceps instability(18,19). This procedure has been used to preserve and stabilise the LHBT. Deepening of the biceps groove, reconstruction of the pulley and ‘tubulisation’ of the tendon have been performed(18). The results have been disappointing, with persistence of shoulder pain and stiffness because of a stenosed, non-sliding tendon, or because of recurrent instability or secondary rupture of the tendon. In a series of 14 shoulders with a subluxed biceps tendon, an attempt at relocation of the tendon and repair of the torn pulley resulted in secondary rupture in 25% of cases(20).
*Tenotomy
This procedure was born out of the observation that spontaneous rupture of the LHBT could alleviate pain in those suffering from LHBT pain. This led some surgeons to develop arthroscopic tenotomy as a simple technique patients significant tendon pain and/or in association with large and irreparable tears of the rotator cuff. This has now become an accepted and common arthroscopic intervention(21,22).
In this simple procedure the LHBT is simply cut and the biceps is ‘let to fly’. It requires no post-operative immobilisation and a short period of rehabilitation when performed in isolation. The disadvantages are the residual deformity, weakness in supination and elbow flexion and sometimes pain or cramping when performing heavy activities. Distal migration of the LHBT after tenotomy may produce the ‘Popeye’ sign. This procedure is used on elderly and low demand patients, and will not be an effective management idea for high-end athletes who need good shoulder function.
*Tenodesis
Tenodesis involves surgically removing damaged tendon tissue and fixing the LHBT onto the humeral head or surrounding soft tissue structures(23). This can be done as an open procedure or more commonly as an arthroscopic procedure using sutures, suture anchors or interference screws. Many variations have been described and several papers have compared the biomechanics of these different methods(24, 25).
The site of tenodesis should be the intertubercular groove of the humerus(26). Other locations are non-anatomical and non-physiologic, and may potentially cause dysfunction of the shoulder and create long-term pain. When a soft-tissue biceps tenodesis is performed in the rotator interval, it is frequently associated with subluxation and will thicken and scar the rotator interval.
Attachment of the LHBT to the coracoid process or the conjoint tendon as proposed in the past with open surgery - and more recently with arthroscopy (Verna) - also changes the course of the tendon and may produce pain caused by traction or adhesions under the insertion of pectoralis major. Richards and Burkhart described an arthroscopic technique for repair of a retracted LHBT rupture(27). The tendon is retrieved and passed retrograde through its anatomical tract, beneath the pectoralis major, and tenodesis is performed in the upper part of the bicipital groove.
Irrespective of tenotomy or tenodesis, it is important to address the intra-articular proximal tendon stump, as it can impinge between the humeral head and glenoid, producing pain and chondral erosion. The free end of the tendon needs to be excised to prevent this.
Conclusion
Injuries to the LHBT are reasonably common in overhead athletes such as swimmers, cross fit athletes and tennis players. They may be injured traumatically in association with other shoulder injuries such as rotator cuff rupture or dislocation, or they may break down due to overload of compression and tension caused by overuse. They may suffer mild inflammation in the younger athletes to more degeneration in older athletes. They may also dislocate and rupture. Treatment for LHBT will depend on severity of the injury, the age of the athlete and the type on use the athlete requires. Tendinitis, tendinosis and tenosynovitis may be managed conservatively whereas rupture and dislocation is usually a surgical issue.References
- Clin North Am 1982;13:453-75.
- J Bone Joint Surg Am 1931;13:160.
- Surg Gynecol Obstet 1939;68:903–17.
- Arthroscopy. 2017 Jan;33(1):28-38
- Am J Sports Med. 1998 Sep-Oct;26(5):610-3.
- J Shoulder Elbow Surg 2004;13:249–57.
- AJR Am J Roentgenol 1983;141:781–8.
- Radiol Technol 1965;37:47–50.
- J Shoulder Elbow Surg 2006;15:7-11.
- J Shoulder Elbow Surg 2004;13:258-65
- Arthroscopy 2001;17:430–2
- Arthroscopy 2002;18:E46.
- South Med J 1979;72:827-30.
- Br J Sports Med. 2015 Oct;49(19):1277-83
- J Shoulder Elbow Surg 1999;8:644-5
- Clin Orthop 1982;163:107-12
- J Shoulder Elbow Surg 2000;9:382-5.
- Arthroscopy 2004;20:964–73.
- Burkhead W. The biceps tendon. In: Rockwood CJ, ed. The shoulder. Philadelphia, Pennsylvania, USA: WB Saunders, 2004:1059–150.
- J Shoulder Elbow Surg 1994;3:353-60.
- J Shoulder Elbow Surg 2005;14:238-46.
- J Shoulder Elbow Surg 2001;10:247-9.
- J Bone Joint Surg Am 1989;71:376–81.
- Arthroscopy 2005;21:764.
- J Shoulder Elbow Surg 2004;13:160-4.
- Knee Surg Sports Traumatol Arthrosc 2007;15:645–8.
- Arthroscopy 2004;20(Suppl 2):201–7.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Further reading
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









