Neck Assessment and Screening
Kay Robinson looks at the mechanics of neck injury and assessment techniques for the clinician.
Nearly half the population will experience neck pain at some point. With sports accounting for around 10% of all neck injuries, the cervical spine is an area that warrants more focused attention than it currently gets(1). The prevalence of neck injuries in sports is thought to be rising, and this is unquestionably partly due to improvements in injury reporting and monitoring. However, the increase in the physicality of sports and the growth of ‘extreme sports’ leave untrained necks at greater risk of injury.
Working in the sport of skeleton (where athletes sprint on ice and then hurtle head first down the icy, often bumpy track at speeds over 130kph) opened my eyes to the importance of neck training. Neck injuries are common in skeleton, so an obvious motivation is to prevent this. However, neck training isn’t just about injury-risk mitigation; in a sport where the gold medal can be decided by a single hundredth of a second, training aimed at strengthening the neck so that it can keep the athlete’s chin off the ice can be the difference between the standing on the podium or applauding from the stands.
To reduce the risk of injury, the neck must be precisely and strategically trained to ensure its tolerance exceeds the demanded loads. However, before implementing this training program, it is necessary to accurately evaluate the cervical spine in a comprehensive assessment and screening process. This will be the focus of the first article of this two-part series on neck injury and the cervical spine.
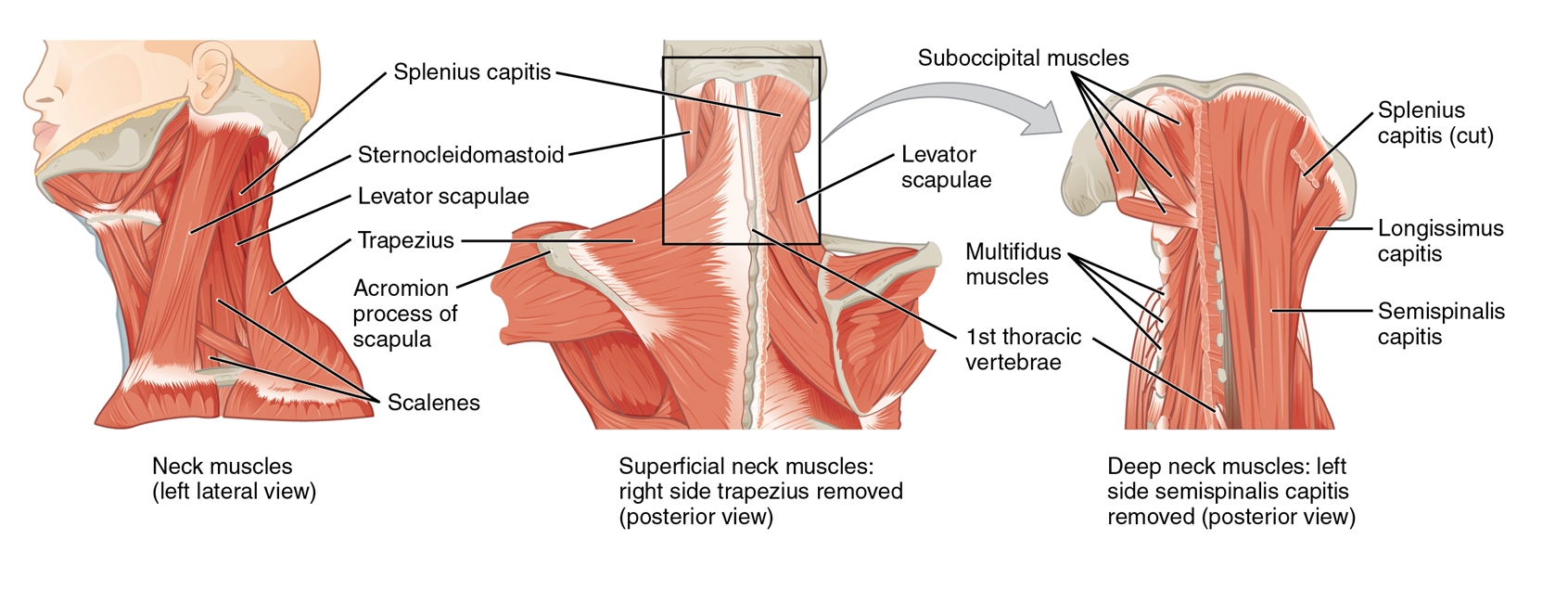
Figure 1: Cervical musculature
How do necks get injured?
Neck injuries are unsurprisingly most common in motorsports and high-impact, collision sports such as rugby. The reasons for this injury profile include:
- Acute force exposure through axial loading (compression and distraction)
- Direct blows
- Sudden acceleration/deceleration
Let’s look at the first mechanism. Compression, or axial loading, is the primary mechanism of neck injuries in sports and most commonly occurs when the load is applied. The neck’s natural lordosis is lost – usually due to excess flexion, causing energy dispersal to be compromised(2). Acutely, the increased loading can cause severe cervical spine trauma, but chronic exposure can also have a cumulative effect. Situations, where this can arise, include collapsed scrums in rugby, falls from heights, and mistimed manoeuvers in combat sports.
Another neck injury that can arise from axial forces is stingers or burners, which frequently result from brachial plexopathy injury or irritation. These can be either compressive or distractive and are most common in tackling sports or due to a fall from a height where the neck is laterally flexed and the shoulder girdle depressed.
Stingers are a result of a downward traction force on the shoulder girdle. At the same time, the neck is contra-laterally flexed or the result of compressive forces that close down the ipsilateral posterior elements of the vertebra. Symptoms are often consistent with a ‘dead arm’ and include temporary altered sensation and weakness due to the irritation of the nerve roots – most commonly of the 7th cervical level(3). Clinicians need to have a high index of suspicion of spinal cord injury following any compression or distraction injury, and this is a severe consequence that needs to be cleared by a thorough on-field assessment before the athlete is moved.
‘Whiplash Associated Disorders’ (WAD) are commonly seen in the general population. However, they can frequently occur in sports involving sudden acceleration and deceleration and can also occur following a blow to the trunk or head(4). A combination of neck pain, headaches, temporal mandibular dysfunction, and referred pain/ neurological symptoms result from the forces transferred to the neck, causing sudden, uncontrolled movement, which damages the anterior and posterior structure of the cervical spine.
However, the cervical spine is not just prone to acute injuries. Chronic force exposure from maintained static positions (such as in sports like archery) or repetitive exposure to gravitational (G) or vibration forces are often implicated in developing overuse symptoms. As with any area of the body, athletes who cannot attenuate the forces they are exposed to through their neck will be at a greater risk of injury or dysfunction.
The side effects of chronic G-force exposure include dizziness, disorientation, altered vision, reduced coordination, and neck pain(5). Any of these side effects can reduce performance and put athletes and opponents at risk, particularly when traveling at high speeds!
Much of the research in this area has been carried out by military air forces, monitoring the effect of G-force on fighter pilots. The symptoms are thought to arise due to reduced blood flow to the head, visual disturbances, and high loads on the neck’s musculature (5).
G-force should also be considered in contact sports, where collisions between players may expose athletes to forces equivalent to those experienced in a car collision(6). Long-term exposure to G-force is suggested to leave athletes at increased risk of vertebral disc degeneration. Therefore, exposure should be monitored closely(7). This is already commonplace in occupational health and safety, where machinery operators have limited time exposure to vibrational forces to minimize long-term damage.
Neck Assessment
In all sporting environments, basic neck range and strength should be assessed to provide baselines and to aid return to sport planning – precisely as we would use following any other peripheral joint injury.
Cervical movement and musculature are complex, with vertebral levels contributing to varying degrees of overall neck motion (see figure 1). The change of orientation of the cervical vertebral bodies of the mid to lower cervical spine allows for rotation, flexion, and extension. However, this also isolates lateral flexion to the upper portion of the cervical spine. When determining the baseline range of movement, it is important to recognize that this commonly decreases with age; therefore, the ‘normal’ range will vary between athletes and is likely to change over an athlete’s career.
The gold standard for measuring cervical range of movement is radiological examination. However, this technique is unlikely to be feasible in the sporting environment due to expense. Many clinicians commonly ‘eyeball’ neck motion, but there are, in fact, several more reliable and inexpensive tools that can be used to increase intra-rater reliability. These include the full-circle goniometer or a tape measure to record the distance between anchor points, which can be easily replicated (see table 1).
The primary stabilizers of the neck are collectively known as the deep neck flexors (DNFs – longus capitus, longus colli, rectus capitis anterior, and rectus capitis lateralis)(8). These are difficult to isolate without using EMG resources but are most active through the commonly prescribed ‘chin tuck’ (craniocervical flexion). The most common assessment used to measure the activation and endurance of the DNFs in the craniocervical flexion test was assessed using a biofeedback device (see Figure 2). This assessment is a valuable baseline test recognizing weakness and movement control dysfunctions. One drawback, however, is that it lacks normalized data(9).
Stabilizers’ activity is significantly decreased and delayed in anyone with neck pain(10). Therefore, this is a great starting point in all neck rehabilitation to regain stability. Postural assessment is also a key component of neck assessment. The primary purpose of the neck is to optimize the head position, and equal displacement of the head’s weight (3-6kg) is essential in minimizing overload to the stabilizing muscles. Segarra et al. describe a battery of reliable tests to aid the assessment of cervical movement control dysfunctions, including neck function in four-point kneeling and with upper limb movement(11).
Table 1: Anchor points used to assess Cx range of movement using a tape measure
| Flexion | Extension | Lateral Flexion | Rotation | |
| Anchor point 1 | Tip of chin | Tip of chin | Tragus of ear | Tip of chin |
| Anchor point 2 | Manubrium | Manubrium | Acromion process | Acromion process |
Prime Movers
Cervical prime mover strength can be assessed in several ways, including using isokinetic and isometric dynamometers. It can be combined with measuring muscle activity using EMG studies to increase validity. Cervical extension is stronger than flexion in general population studies, while lateral side flexion is commonly coupled with extension with a bias towards the subject’s dominant side. In athletes who rely on a dominant side bias (e.g., racquet and throwing sports) for performance advantage, this asymmetry should be recognized but not necessarily considered detrimental.
In the athletic environment without access to isokinetic and EMG equipment, baseline strength can be determined using a handheld dynamometer, ideally mounted to minimize assessor bias. Decisions on which ranges should be tested should remain consistent and accommodate for sport-specific positions if required.
To ensure data is normalized, the following considerations should be made:
- Torso stabilized
- Minimized lower limb involvement (e.g., feet on wobble cushion)
- Set appropriate ranges that strength will be measured at/through
- Standardized warm-up and testing protocols
The neck does not function in isolation. Strong correlations have been found between neck pain and shoulder dysfunction and vice-versa; therefore, neck assessment should also consider the entire kinetic chain. With swimmers in particular, shoulder dysfunctions commonly lead to hypertonicity of the cervical muscles, resulting in muscle imbalances, dysfunction, and pain, all of which predispose the athlete to further neck injury(12).

Figure 2: Craniocervical flexion test(13)
The craniocervical flexion test (see figure 2):
- Patient supine, crook lying with the neck in a neutral position.
- An uninflated pressure sensor is placed behind the neck to border the occiput.
- Inflate cuff to 20mmHg.
- Movement is described as a slow head-nodding action.
- Patient attempts to sequentially target five 2mmHg progressive pressure increases, with 10sec holds.
Compensation strategies to observe:
- Pressure loss of > 2 mmHg.
- Began using superficial neck flexors (palpation).
- Jerked chin down.
- Loss of cervical lordosis through retraction.
Neck injuries and concussion
Clinicians should have a high level of suspicion of concussion when treating acute neck injuries due to the high forces translated between the areas. It follows from this: neck assessment should be carried out in all athletes following concussion or head trauma. As research into concussion grows, there is more focus on the association with neck strength. Collins et al. concluded that neck strength was a significant predictor of concussion amongst a large sample of high school athletes and, although further research is needed, showed positive outcomes in reducing concussion risk from adopting neck strengthening programs(14).
Summary
Cervical injuries can occur in a range of sporting environments from the result of acute trauma through axial loading, prolonged position exposure, whiplash, and external forces such as vibrations and G forces. All cervical assessments should rule out severe spinal injury and concussion and also include a range of movement measurements and deep neck flexor and prime mover strength assessment. Consideration should also be made for the rest of the kinetic chain – in particular, the shoulder girdle – due to the high correlation between dysfunctions of the two areas.
In the next article, we’ll discuss management ideas for neck injuries and the phases of rehabilitation, whether it’s to return players to the field post-injury or address any dysfunctions found in assessment and screenings.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









