Tendinopathy: new thinking on an old problem

Tendinopathy is the most common overuse injury in sport and is a concern to both recreational and competitive athletes. More susceptible sports are those that involve prolonged running or jumping actions and high levels of repetitive loading(1).
Tendons comprise the end point of a muscle and attach the muscle to the bone. Their role is to transmit the force of the contracting muscle to the bone and control movement. Movement is controlled by the storage of elastic energy within the tendon. Tendons are composed of collagen bundles - predominantly type I collagen - which can withstand significant tensile loadings.
When the force applied to a tendon increases or becomes significantly repetitive over time, the build-up in mechanical loading to the tendon induces stress in the tendon tissues and causes small tears in the fibers. There is an increase in type III collagen (which cannot withstand load-bearing capacity like type I fibers can). The result is that the tendon reaches a point of failure earlier in response to this mechanical loading(2). Continued overuse causes these tears to become larger, until it weakens beyond failure, causing more tearing, and finally pain (see figure 1).

If the tendon is continually subjected to overload, it will attempt to protect itself by bringing new cells to the area, causing further thickening. The collagen matrix becomes a disorganized mass of cells, which leads to tendon disrepair and cell death rather than repair. Pathologically, the tendon is a mix of healthy tissue interspersed with damaged and dead cells. The ability of the tendon to heal despite the chaos occurring in the tissue depends on the extent of the degeneration process. Management of a diseased tendon requires a comprehensive understanding of the adaptations to identify how symptoms can be reduced(3).
Initial tendinopathy management
The early stages of tendon pathology management (reactive or early disrepair stages) require a prompt reduction in pain and diffusion of the injury to prevent further tendon damage. It is now speculated that inflammation is not the cause of the pain; instead, it is in fact due to the damage to the tendon fibers, which causes an influx of cells to the region, resulting in tendon swelling. Where there is swelling, excess fluid will accumulate, and any stretching of or compression on the tendon will result in a painful response. Avoiding stretching and compression is achieved by keeping the tendon held in a relaxed position. In the case of Achilles and peroneal tendons, for example, this can be achieved with the use of heel raises.Load management can commence from the time of injury. Indeed, it is important to introduce loading early on because complete removal of tendon loading is detrimental to repair mechanisms. Isometric loading has been shown to induce an analgesic response following tendinopathy by causing a reduction in cortical inhibition(4). This means that isometric loading temporarily alters the pain perceived by the brain, which allows the athlete to apply load to the tendon without pain. Isometric exercises should be completed in the mid-range of the muscle motion so as not overstretch or compress the tendon. Application is suggested to be for a loading duration of 4-60 seconds, performed four to five times per day(4).
Conventional thinking on eccentric loading
Management of tendons in the late disrepair or degenerative stage has seen an abundance of recent theoretical research. Previously, eccentric loading (when the muscle is working while lengthening - as opposed to concentric actions where the muscle shortens when working) was the gold standard of treatment. This is why eccentric exercise has been widely accepted as the principal of treatment for tendinopathy (see box 1). However, advances in research have recently emerged.
Recent advances in tendinopathy management
Recent studies have investigated using alternative methods of strength training to load tendons. The aim remains the same: to load the tendon adequately enough to create structural adaptation and therefore recovery from injury, but the methods behind it differ.1) Heavy, slow resistance training (HSRT)
Heavy, slow resistance training (HSRT) involves using high loads upon the tendon, such as 70-85% of one repetition maximum (RM). This is the most weight someone can lift for one repetition, and therefore suggests a significant amount of loading to the tendon. This proposed protocol suggests starting with a more manageable load, e.g., that of your 15RM but with higher repetitions of 3 x 15, and then each week, increasing the load and decreasing the repetitions(9).
This form of exercise allows the tendon to be subjected to greater volumes of loading with fewer repetitions. This results in a greater time under tension, leading to greater tendon adaptation(8). The way by which this occurs is thought to be due to the HSRT causing changes in the fibril morphology and creation of new fibrils (a fibril is a small component that makes up a muscle fiber), therefore adapting the tendon towards a normal morphology(10).
2) Combined loading program
Another theory suggests that rather than using only one form of strength training for tendons, why not combine them and issue a collective approach of loading the tendon? The combined loading method involves loading the tendon concentrically, eccentrically, and then with faster loading by introducing aspects of power and plyometrics type exercises(11). This appears a logical approach to reflect correct tendon function; during sporting activities, tendons will experience all of these types of loading.
The combined loading program was adopted to allow athletes to continue sporting activities, including running and jumping, as long as their pain levels were monitored and did not exceed 5 out of 10 on the pain scale. This program provides a continual loading program to the tendon, while sports are still practiced. Results show that there is no detrimental effect on the tendons, suggesting the continued loading - if monitored correctly, is appropriate for tendinopathy treatment(11).
How are these principles applied clinically?
Each of these methods of tendon loading- eccentric, heavy slow resistance, and the combined program -all load the tendon adequately to initiate tendon adaptations. However, how they are prescribed clinically varies. Figure 2 details the clinical differences and applications of these methods for Achilles tendinopathy
| Treatment for Achilles tendinopathy | Eccentric loading | Heavy slow resistance training | Combined loading programme |
|---|---|---|---|
| Original research | Alfredson et al. 1998 | Kongsgaard et al. 2009/2010 | Silbernagel et al. 2007 |
| Type of exercise examples | 2 styles of heel drops; first with a straight knee, and then with a bent knee | Seated calf raises, heel raises on the leg press machine, standing calf raises with barbell | 2-legged calf raises, 1-legged calf raises, seated calf raises, eccentric loading, quick rebound & plyometric exercises |
| Prescription | Eccentric loading | Eccentric and concentric loading | Concentric and eccentric loading, as well as power and plyometric loading |
| Load | Three sets of 15 repetitions | 70-85% of 1RM | Start with body weight and increase load as able each week in three sets of 15-20 repetitions |
| Frequency | 2 x per day | 3 x per week | 1 x day |
| Duration | 12 weeks | 12 weeks | 12 weeks to 6 months |
The pros and cons debate
Each technique discussed above is known to remodel the injured tendon physiologically, and result in positive research supported outcomes. So how do we decide which method to adopt? Eccentric loading does create pain and is often not introduced at the initial stage following injury. Instead, rest until the pain subsides and begin loading as tolerated following the recommended loading dosage.Both the HSRT and the combined loading programs, however, allow treatment to commence immediately, therefore giving control to the athlete and allowing physiological adaptations to occur earlier. These two methods could have a greater appeal to the active athlete who does not want to rest from training. The combined loading program, in particular, would appeal because it approves of continued loading in the form of running and jumping. This can help athletes to continue to use their specific sport and skills - as long as pain levels are monitored. Also, a prohibition from training can be a barrier to psychological recovery, confidence, and delay time off of the sport.
The eccentric program requires the greatest total loading time to the tendon in a week, with 308 minutes required, compared to 107 minutes per week for the HSRT program (9). Patient compliance was found to be significantly higher with the HSRT plan as a result. Interestingly, patient satisfaction was rated at 100% after 12 weeks of the HSRT plan compared to 80% with the eccentric loading(9). These figures were similar when measured again at 52 weeks, suggesting greater compliance is linked to greater satisfaction, likely because the clinical outcomes were better with increased adherence.
Both the HSRT and combined loading programs allow for greater control over the tendon loading. They both suggest that loading should be increased weekly as tolerated, therefore allowing applications to be tailored to the athlete. Their guidelines also better reflect those of strength building protocols, where the American College of Sports Medicine stated that for optimum strength gains, loading should be between 8 and 12 reps max, with three sets of 8-12 repetitions, repeated 2-3 times per week(12).
Be patient!
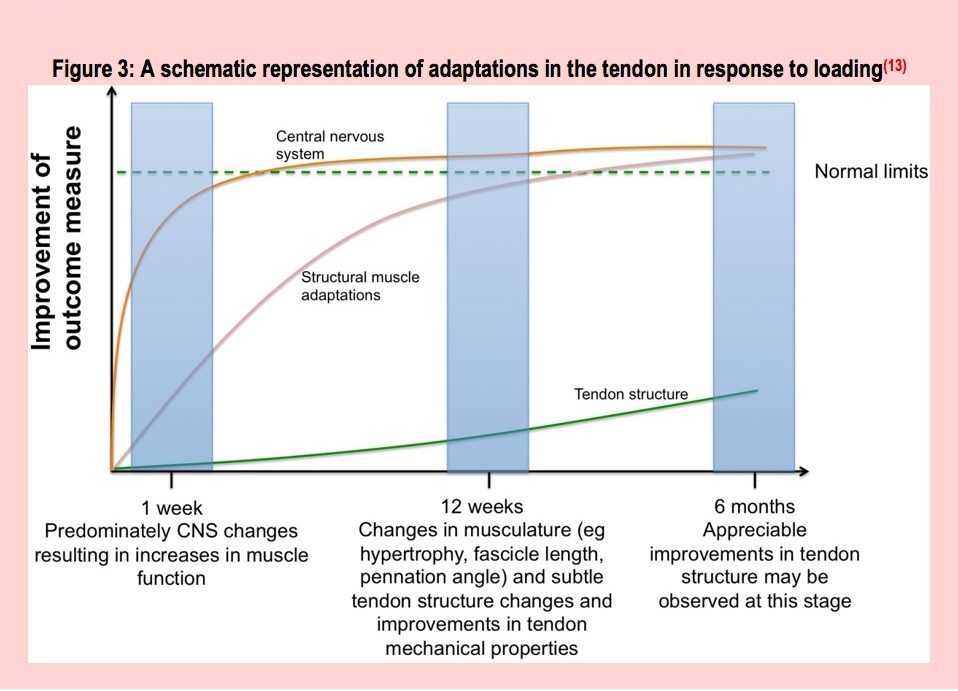
The key to successful tendon rehabilitation is appropriate load management for the tendon. The tendon’s capacity is only increased if it meets the demands of the load placed upon it. This progressive loading initiates the adaptation to the tissue, and hence its recovery. This process cannot be accelerated or achieved with a quick fix. All of the different research methods we have discussed have the same principle in common; the loading programs take a minimum of 12 weeks. This is due to the physiological changes that have to occur for tissue adaptation (see figure 3).Initial changes that occur with isometric loading predominantly affect the central nervous system and the brain’s response to pain; with continued loading then affecting the muscle-tendon system and causing the structural adaptations (see figure 3). Note that at 12 weeks there are “improvements” in the tendon and at six months “appreciable improvements.” This is important to consider for long-term rehabilitation. Tendon loading must continue regularly beyond initial rehabilitation and return to sport, to ensure the tendon continues to withstand the demands of competition. Should rehabilitation stop too early the tendon is at risk of re-injury.
Figure 3: A schematic representation of adaptations in the tendon in response to loading(13)
Summary
Here are the key points for clinicians to bear in mind when rehabilitating athletes with tendinopathy:- Initial tendon management should consist of avoiding stretching and compression, and application of isometric exercises for 40-60 second 4-5 times per day. Ibuprofen can also be taken.
- Strengthening is the primary treatment of tendinopathy, and there are now several supported methods including eccentric loading, heavy, slow resistance loading, and a combined loading approach.
- Gold standards suggest progressive loading is paramount. The load must be progressed to the level at which the tendon will be exposed, ie, enough to cope with the load and force of repetitive running or jumping, etc. Exercises should progress by increasing the load applied and decreasing repetitions as required.
- Power and plyometric exercises must be added for high-level rehabilitation to ensure the tendon can store energy and produce the forces required without pain or weakness. This is essential for a return to sport and should be continued long-term beyond six months post-injury.
References
- Phys Ther in Sport. 2012 June; 13:3-10
- Clinics in Sport Med. 1992 11(3); 601-624
- Br J Sports Med. 2009; 43(6): 409-416
- Br J Sports Med. 2014; 48: 506-509
- Phy Ther in Sport. 2000 1; 6-14
- Phy Ther in Sport. 2007 8; 191-196
- Phy Ther in Sport. 2007 8; 88-97
- Sports Medicine. 2013; 43(4), 267-286
- American J Sports Med. 2015; 43(7): 1704-1711
- American J Sports Med. 2010; 38:4, 749-756
- American J Sports Med. 2007; June 35(6): 897-906
- American College Sports Med. 2009; 688-708. DOI: 10.1249/MSS.0b013e3181915670
- Br J Sports Med. 2018; 52(10): 622-623
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.






