Four necessary traits for building better patient/clinician relationships

Being in pain, out of work, or away from training can be both physically and psychologically debilitating and detrimentally affect a client’s entire well-being and lifestyle. An alliance between the patient and therapist is essential for beneficial therapeutic outcomes(1). How exactly to achieve this beneficial relationship is a challenge to clinicians with packed schedules and administrative expectations.
The nature of the challenge
The first reference to an ‘alliance’ within a therapeutic situation was in 1912 by Freud, who referred to a sense of collaboration, warmth, and support between a client and therapist(1). Later in the 1970s, Bordin described three factors constructing the alliance as follows(1):
- The therapist-patient agreement on goals of treatment;
- The therapist-patient agreement on interventions;
- The affective bond between the therapist-patient.
Clinicians must determine treatment goals and the interventions to reach them, with sensitivity and accuracy. The clinician who builds a good rapport with their patient positively affects attitudes and behaviors and encourages them to engage in their therapeutic journey(2). The nature, severity, and irritability of an injury are unique to each individual, which means it’s not just the treatment modality used to treat them that’s important, but also the manner and tone used to do so.
Research findings
Researchers from the University of Sydney conducted a systematic review assessing whether the working alliance is related to the outcomes within physiotherapy practice(1). The authors identified 13 associated papers, six of which pertained to musculoskeletal conditions (3/6 related to the low back, 1/6 related to the neck, and 2/6 having multiple diagnoses of musculoskeletal complaints). The review found significant positive associations between the alliance and the patients’ perception of the treatment, change in pain, physical function, patient satisfaction, depression, and general health status.Researchers from the University of Alberta carried out a qualitative study looking at the conditions required to develop an alliance between a physiotherapist and a patient(3). They recruited eleven physiotherapists, all of whom had a minimum of ten years’ clinical experience in private practice, and seven patients (four male), to provide detailed accounts of their appointments. Six patients had previous physiotherapy treatment and five patients had symptoms for more than three months. The investigators interviewed the patients about their therapeutic experience.
The interview data revealed four specific traits exhibited by the physio that improved the patient and therapist relationship. These were being:
- Present
- Receptive
- Genuine
- Committed
Consider these traits as a box, whereby being present forms the base and provides support for receptivity, commitment, and genuineness to occur – ie, the walls of the box (see figure 1). This framework offers a structure for a successful patient/therapist interaction during an appointment. When a therapist exhibits these traits, they can successfully collect the specific details of the injury and medical history from the patient, and place them inside the box. The patient feels part of a partnership, and they collaborate to work within this framework.
Figure 1: Framework for relationship building
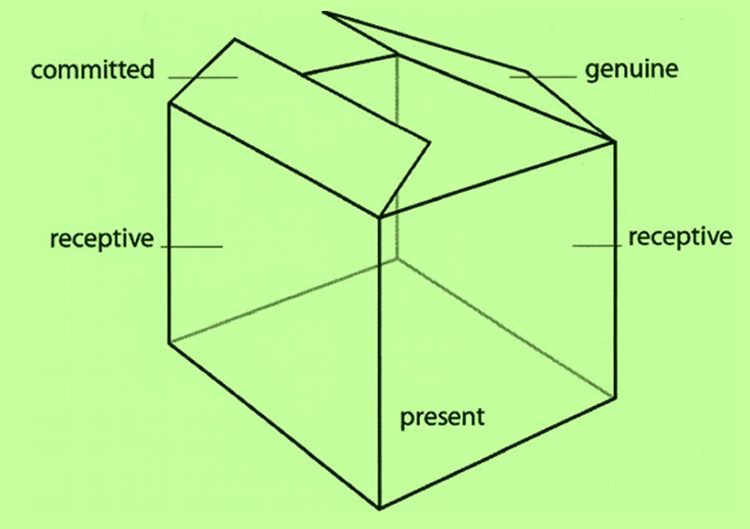
The four traits on which to forge an alliance between the therapist and patient.
Practical advice for clinicians
It is crucial to implement these guidelines in practice to enhance the patient’s therapeutic outcomes. These practical guidelines focus on each of the four characteristics, all of which facilitate the foundation upon which to build the therapist/patient relationship and improve patient satisfaction and outcomes.Being present
- Patients notice and appreciate when a therapist spends extra time with those who need it. This patient attention gives the impression that time is of no consequence, and the therapist is willing to do what is necessary to address the issue. Of course, this isn’t always possible or ideal, but if the schedule allows, extra time spent with a patient is well worth it in the patient’s eyes.
- Patients are aware when a therapist is rushing or distracted by other things going on in the clinic environment. The patient places importance on creating a bubble whereby the sole focus is on the patient and their appointment.
Being receptive
- Patients report that telling their stories is important and creates a safe environment where they feel heard. It is all too easy for a physiotherapist to presume aspects of the situation based on the diagnosis. Therefore, it is important for a therapist to have an open mind going into an appointment instead of a pre-planned structure they need to follow.
- At the same time, the patient also needs to listen and receive the ideas that the physiotherapist proposes with an open mind.
- A patient’s body language or tone of voice may reveal information about other relevant issues they are hesitant to bring up. Identify verbal and nonverbal cues to better understand and relate to the patient.
Being genuine
- It is important that a therapist presents a warm and personable manner within an appointment. This demeanor facilitates authentic and sincere responses from the patient.
- Transparency from the patient about the history of the condition and from the therapist regarding the treatment and rehabilitation plans are important.
- Use clear and direct language. Temper tone with compassion while being as straightforward as possible and providing a firm plan of care.
- Reveal something personal about yourself to develop a bond. Some patients benefitted from knowing their therapist on a more human level, but remember not to cross the line of professionalism. Consider what you and the patient might have in common and talk about that.
- Learn about the patient’s lifestyle to reveal the cause of the problem and tailor a plan with which they will be compliant.
- Remember small details about the patient’s life or circumstances (eg the names of their family members or pets, etc.) to strengthen the client-patient bond by making the patient feel unique and significant.
Being committed
- The therapist must commit to understanding the needs of the patient through careful questioning and listening.
- The patient, too, must commit to helping themselves for an effective therapeutic experience.
- Patients report understanding the physiology of their injury, helps them understand the rationale for their treatment course. However, while patient education is a good thing, realize that not all patients have the desire to understand their physiology.
- Clinicians demonstrate commitment and compassion by considering all the factors that affect patient care. Patients perceive them as going the extra mile to enhance their care.
- Patients report that seeing the same therapist throughout their course of care is an essential aspect of their ongoing treatment and shows commitment on the part of the therapist.
In summary
While clinicians can deliver the most up-to-date and scientifically-based treatment, ignoring the tone and manner in which they do so will affect patient outcomes. Fostering an environment in which the patient feels cared for through presence, receptivity, commitment, and genuineness, allows for a beneficial patient/therapist relationship. A therapist may have dozens of patients on their roster, but in the patient’s eyes, there is only one therapist. Importantly, the things a physiotherapist says and does have a significant effect on a patient’s well-being and psyche – perhaps more than they will ever know.References
- Phys Thera, Aug, 2010, 90, 8, 1099-1110
- Int J of Physio, 1997, 13, 1, 89-96
- Arch of Physio, 2018, 8, 3, 1-12
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










