A hop, skip, and a jump: restoring function following surgical repair of patellar tendon ruptures

With an incidence of 0.6%, a healthy patellar tendon rupture is rare(1). Patellar tendon ruptures (PTR) are often the result of trauma (direct or indirect) or tendon degeneration(2,3). The typical mechanism of injury for a PTR is an eccentric contraction of the quadriceps while the knee is partially flexed in a closed-chain position(3). A PTR typically occurs in young, active individuals under 40 (see figure 1) (2).
Figure 1: Anatomy of the patella
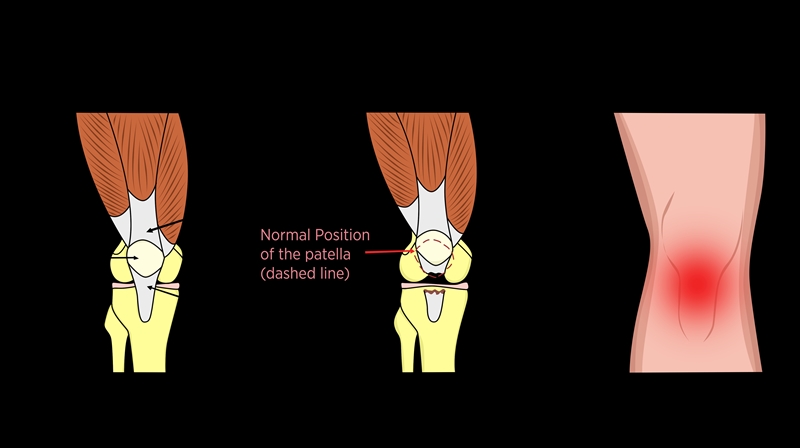
The patella is a sesamoid bone that lies within the common quadriceps femoris tendon. The common location of a PTR is at the infrapatellar osteo-tendinous junction and presents with anterior knee pain and swelling(2).
Warning signs
Compared to quadriceps tendon ruptures (QTR), PTRs occur less frequently. Although the typical mechanism is due to trauma or degeneration, a spontaneous rupture may result from local steroid use or metabolic diseases such as diabetes mellitus, renal failure, and systemic lupus erythematosus(1). The metabolic disease causes local vascular damage and may lead to tendon disrepair and degeneration, which affects the tendon's capacity to withstand load adequately and increases the risk of a rupture. The forces required to overload the patellar tendon are 17.5 times body mass. Yet, a continuous subthreshold load may cause microtrauma and lead to reactive and degenerative tendinopathy(1). Jumping and landing are activities that place a substantial load on the tendon. Due to the open epiphyseal plates, adolescents are prone to avulsion fractures rather than tendinopathy(1).A common autograft to reconstruct the anterior cruciate ligament (ACLR) is the central third of the patellar tendon. A PTR following bone-patellar tendon-bone (BPTB) ACLR is rare, but cases do exist. Devascularization, poor tendon healing, and trauma at the time of harvest are potential contributors to tendon failure after ACLR(4).
Clinical Presentation
In acute PTR, it is essential to determine the mechanism of injury and tendon health history. Immediate swelling, anterior knee pain, loss of knee flexion range and extension strength, and the inability to bear weight are all hallmarks of a significant knee injury. However, PTR patients may present with a proximally displaced patella and a palpable infrapatellar defect(1). Imaging in the form of an MRI remains the gold standard for diagnosing PTR. However, an x-ray can rule out differential diagnoses such as a patella alta, tibial tuberosity fracture, or patella or tibial tuberosity avulsion(2).Conservative or surgical intervention?
Full-extension immobilization (for up to three weeks) is recommended for an incomplete PTR with a functional extensor mechanism(2). The best outcomes for complete PTR result from surgical intervention within seven days post-injury(2). A suture technique ensures adequate tension, correct position, and patellar tracking (see figure 2)(2).Figure 2: Patellar tendon repair
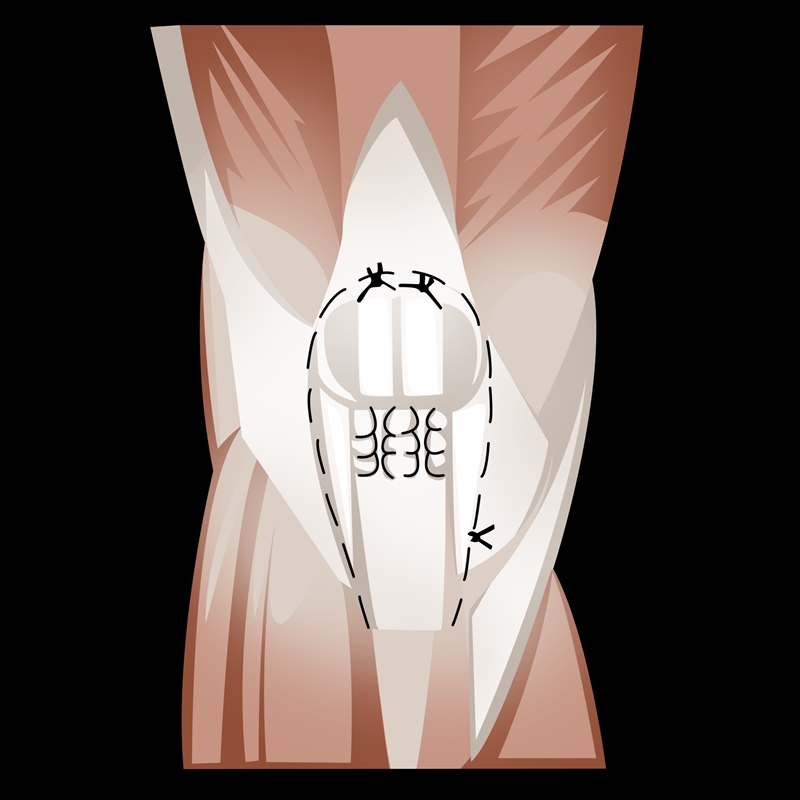
Most ruptures occur at the osteo-tendinous junction and require a trans-osseous suture technique. An anterior approach through a midline incision allows for accurate dissection of the retinacular tear and tendon debridement. The surgeon decorticates the inferior pole of the patella and sutures the repair(2).
Rehabilitation
Without adequate long-term follow-up, the debate around early versus delayed mobilization post-operatively remains unsolved in the literature. Immobilization in the initial weeks prevents the sutures from failing(5). On the other hand, early mobilization reduces joint stiffness and adhesion formation and improves bone density, cartilage preservation, and muscular strength(6). An early mobilization program that consisted of progressive continuous passive movements (CPM), weight-bearing as tolerated, and isometric quadriceps strengthening displayed excellent functional outcomes(6). Despite the apparent benefits of early mobilization, delayed mobilization does achieve good functional and return to sport outcomes(1).Investigators at the Naval Medical Center in Virginia compared a delayed and early mobilization program following patellar tendon repair(7). After a minimum of 16 months of follow-up, the results were mixed with no difference between groups. The degree of function, pain, and muscle strength was not dependent on the intervention. Researchers at Ibn Rochd University in Morocco investigated the long-term outcomes of an early mobilization and strength program following PTR repair (see table 1)(8). They identified positive functional results and significantly reduced pain at follow-up(8).
| Phase 1 | 0- 2 weeks | Initial mobilization in a brace between 0-30 degrees |
| Mobilization between 0-60 degrees in week two | ||
| Closed kinetic chain isometric quadriceps strengthening (full weight bearing) | ||
| Phase 2 | 2-6 weeks | Passive knee flexion was limited to 90 degrees (no active knee extension) |
| Continue isometric strengthening | ||
| Phase 3 | 6-12 weeks | Progress isometric strengthening |
| Introduce unresisted active extension | ||
| Introduce active flexion to 90 degrees | ||
| Phase 4 | 12-16 weeks | Full range of movement |
| Introduce progressive step up exercise | ||
| Avoiding forceful eccentric contractions | ||
| Phase 5 | 16-24 weeks | Introduce functional rehabilitation exercises, including low intensity closed kinetic chain exercises |
| Phase 6 | 24+ weeks | Progress functional rehabilitation and increase intensity |
| Introduce graded plyometric and sports specific activities |
Conclusion
Patellar tendon rupture is a rare occurrence when compared to other sporting injuries. However, understanding the risk factors, mechanism of injury, and rehabilitation options is important to guide best practice. Health promotion and education on using local steroids and managing metabolic disease are essential for preventing tendon ruptures. Rehabilitation through delayed or early mobilization does not appear to affect long-term functional outcomes. Thus, with the additional benefits of early mobilization, it seems safe and viable with no greater risk of disrupting surgical repair integrity. With the range of surgical repair options, clinicians should always consult the surgeon for specific rehabilitation guidelines.References
- Injury, Int J Care of the Injured. 2017;2515-2521.
- Asia-Pacific J of Sports Med, Arthro, Rehab and Tech. 2015;2 (4): 99–107.
- Scan J of Surg. 2016;105(2): 67-72.
- Am J of Sports Med. 1996;24(5): 698-701.
- Orthop & Trauma. Surg & Res.2015;101: 307-311.
- Injury, Int J Care of the Injured. 2003;35: 76–79.
- Arch Phys Med Rehabil. 2000;81:786-8
- Annals of Phys and Rehab Med. 2017;60(4): 244–248.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









