Brachial plexus injuries in the athlete

Brachial plexus injuries (BPI) are a reasonably common injury in contact-sport athletes. These are typically referred to as ‘stingers’ and ‘burners’, and represent a transient and reversible peripheral neuropraxia of all or some of the nerves (usually the upper trunks) that comprise the brachial plexus. These stretch and/or compression injuries result in transient radicular pain, paraesthesia, numbness, and weakness in the arm. Rarely, these nerve injuries may be severe and result in avulsion or rupture of the nerves.
Relevant anatomy
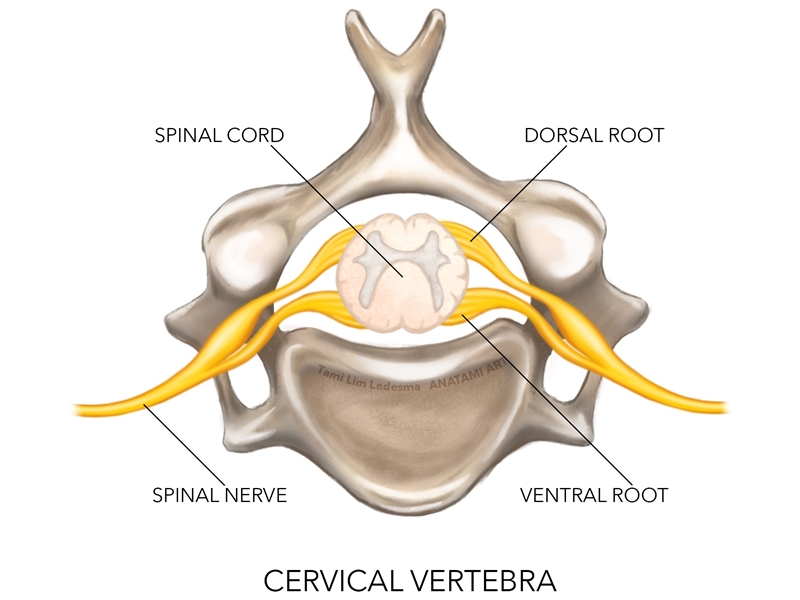
While a complex anatomical arrangement, the important points to note regarding the brachial plexus and its relationship with other supraclavicular structures are as follows (see figure 1):- It is formed by the ventral rami of C5-C7 and T1, with variants occasionally coming from C4 and T2.
- C5 and C6 form the upper trunk.
- C7 forms the middle trunk.
- C8 and T1 form the lower trunk.
- Above the clavicle these trunks divide to form the posterior, medial and lateral cords and these are named due to their relationship with the subclavian vessels.
- From the cords, the primary peripheral nerves of the arm branch out to form the musculocutaneous, axillary, radial, median and ulnar nerves.
- The smaller peripheral nerves such as the long thoracic, suprascapular and dorsal scapular nerves arise from the roots, trunks or cords.
For a more detailed description of the anatomy of the brachial plexus, the reader is directed to the work of Bonham and Greaves 2011(1).
Figure 1: Brachial plexus complex
Epidemiology
BPI can be caused by a wide variety of mechanisms. These include(1):- Falls
- Traumatic traction
- Crushing and penetrating injuries
- Obstetric complications
- Thoracic outlet syndrome
- Other causes such as tumors, aneurysm of the underlying vasculature, or secondary compression due to malunion of the clavicle (Bonham).
Traumatic non-sporting injuries usually involve adults who suffer a fall and either dislocate a shoulder or fracture the neck/head of the humerus. These usually only involve the inferior trunks of the brachial plexus. The other common group involves motorbike or cycling injuries where the arm undergoes a sudden and violent traction caused by an accident/fall. Traumatic non-sport injuries are often the more severe as the velocities involved (such as a motorbike accident) can be quite large.
In the sporting context, contact-sport athletes comprise the largest group of athletes who suffer from BPI. It has been suggested that 50-65%(2)of American football players and 30-40%(3)of rugby players have suffered a ‘stinger’ or ‘burner’ at least once. However, it has been suggested that the incidence may, in fact, be much higher as athletes will often not report these injuries to medical staff because the majority subside within 24 hours. In addition, the advent of the cervical roller used by American Football players may reduce the severity of these injuries as it protects the cervical spine from excessive side flexion mechanisms of injury(4).
The usual mechanism of BP injury is closed trauma due to a direct blow, compression or traction (see figure 2).
- Direct blow injuries are rare and are caused by a percussive mechanism to the cords and trunks. This would be a result of direct contact with a ball or implement such as hockey stick or in combat sports.
- Compression injuries of the roots are caused by forced ipsilateral cervical lateral flexion and/or extension that narrows the intervertebral foramen and compresses the nerve root.
- The more common traction injuries are caused by a sudden stretch on the nerve caused by contralateral side flexion of the cervical spine and/or sudden depression of the shoulder girdle. This would be typically caused by tackling another player or landing suddenly on the point of the shoulder and the head and neck laterally flexing away(5,6).
Figure 2: Usual mechanisms of BP injury
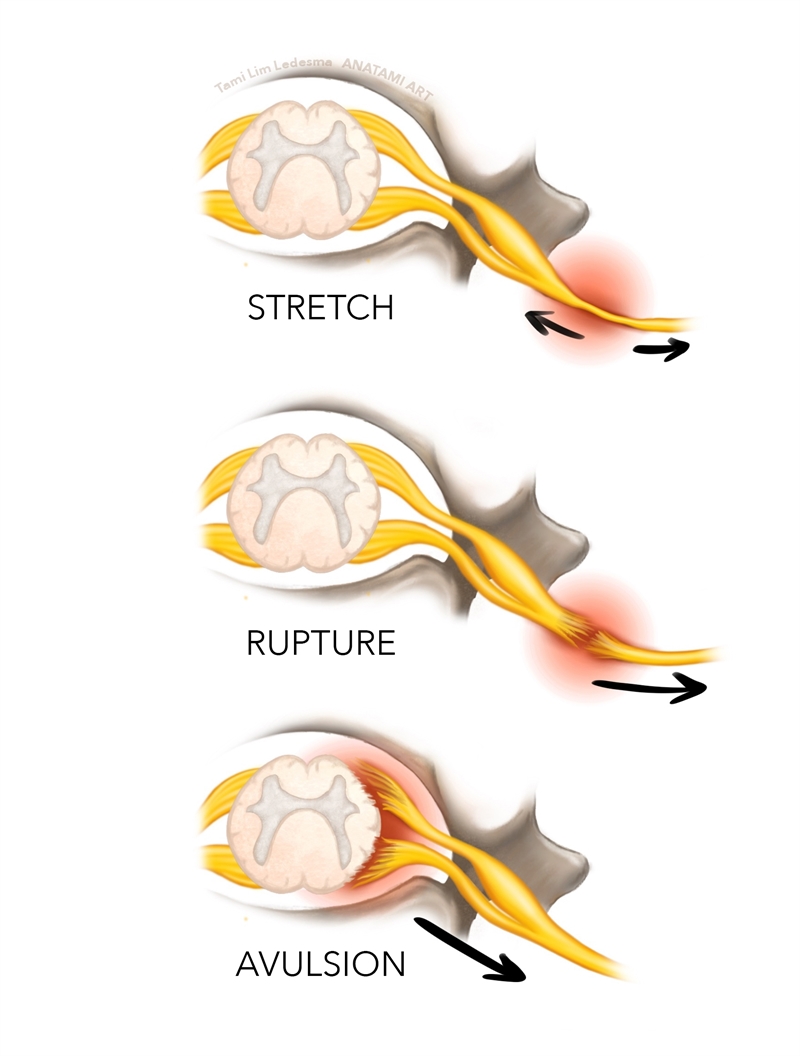
Traction injuries due to contralateral side flexion on a depressed scapular typically lead to stretching of the upper brachial plexus between two fixed points, resulting in either avulsion, rupture or stretch of the upper roots (C5, C6, C7) with preservation of the lower roots (C8, T1). Alternatively, BPI traction may also be caused by sudden traction with the arms overhead such as gymnast, or Crossfit athlete, who suddenly grabs a bar overhead as the bodyweight is falling. This would more commonly lead to lower brachial plexus injuries (C8–T1).
Finally, traction-related BPI can be seen when there has been a forcible widening of the scapulohumeral angle (due to shoulder dislocations or fractures of the humerus). This causes tension on the infraclavicular neurovascular bundle over the humeral head, with the potential for rupture or damage to the infraclavicular plexus (7).
Pathogenesis
Traction injuries to the brachial plexus may result in one of the following three sequelae:- A stretch of the nerve root (leaving it in physical continuity).
- A rupture of the nerve root (two stumps will then be available for repair).
- An avulsion of the nerve root from the spinal cord (no proximal stump available).
The rupture and avulsion types of injury are usually the result of severe trauma (eg high-speed motorbike accidents), with contact-sport athletes more likely to suffer lower grade stretch based injuries.
In more severe avulsion and rupture scenarios, root avulsions are present in 75% of cases, with the roots and trunks being the most commonly injured sites(8). Root injury is defined as root avulsion from the spinal cord or a rupture in the preganglionic root zone at the vertebral foramen. Injuries distal to the ganglion are classified as a post-ganglionic injury, which divides into supra and infraclavicular injury. Post-ganglionic supraclavicular injury includes injury of the spinal nerves, trunks and the divisions. The post-ganglionic infraclavicular injury involves injury of the cords and the terminal branches. Given that there is little potential for recovery without surgical reconstruction for preganglionic injuries(9), diagnosing whether a brachial plexus injury is a pre or postganglionic lesion is critical when considering the possibility of spontaneous recovery. Postganglionic lesions have the potential for recovery, depending on the severity of the injury (discussed in part two).
The role of the cervical spine
The cervical spine has a few unique anatomical features that may act as a protection against repetitive traction type injuries. The free mobility of the nerve sleeve, ganglion and spinal nerve within the foramen, allows the neural structures to adapt to movements of the cervical spine without deformation or injury. Furthermore, the spinal nerves and the transverse process adhere to the level of the lower cervical spine. When traction force affects the spinal nerve, this adherence of the spinal nerve and the transverse process protects the nerve root to spinal cord connection. For these reasons, a considerable force on the shoulder and upper arm is required to carry sufficient power to cause root avulsion, and this may explain why these are not common in contact sports.Classification of injury
The original classification of BPI was initially presented by Seddon in 1943(10)and expanded by Sunderland in 1951 (11). This is summarised below in table 1.| Sunderlandclassification | Seddon classification | Pathology | Motor paralysis | Sensory paralysis | Muscle atrophy |
|---|---|---|---|---|---|
| 1 | Neuropraxia | Conduction block | Complete | Minimal | Minimal |
| 2 | Axonotmesis | Transection of the axon with intact endoneurium | Complete | Progressive | Complete |
| 3 | Axonotmesis | Transection of the nerve fibre inside, and intact perineurium | Complete | Progressive | Complete |
| 4 | Axonotmesis | Transection of the funiculi, nerve trunk continuity being maintained by epineural tissue. | Complete | Progressive | Complete |
| 5 | Neurotmesis | Entire transection of nerve trunk | Complete | Progressive | Complete |
| Root avulsed | Root avulsed | Root avulsed from spinal cord | Complete | Progressive | Complete |
The key features of the types of nerve injuries are:
Neuropraxia:
- Conduction block with transient demyelination.
- Recovery is spontaneous
- Wallerian degeneration does not occur.
Axonotmesis:
- Disruption of the axon within an intact nerve.
- Wallerian degeneration in distal segment of the nerve.
- Recovery at a rate of 1mm/day.
Neurotmesis:
- Complete disruption of the nerve.
- Recovery not possible without surgery.
In the contact-sport athlete, most BPIs are the grade/type 1 variety (neuropraxia) with most athletes recovering within three weeks(12). The more severe injuries (grade 2) may take 10 to 12 months to heal since these injuries are a combination of neurapraxia and axonotmesis.
Signs and symptoms
BPI is characterized by:- Presence of burning pain radiating from the neck down the unilateral arm and hand.
- A ‘dead arm’ type sensation whereby the athlete feels unable to use the arm for a short period of time.
- Usually last for seconds to hours, rarely persisting beyond a 24-hour period.
- Athletes may experience associated weakness of the muscles, which typically resolves within 24 hours to six weeks after injury. Based on the clinical presentation of stingers, the C5-C6 nerve distribution is generally most frequently affected(13).
On-field/in-clinic examination requires a thorough examination of muscle power and skin sensation to determine the root, trunk and cord involvement. The simplest way to ascertain the level is to assess the following(14):
- Inability to abduct the arm (C5).
- Weak elbow flexion and wrist extension (C6).
- Wrist and forearm weakness (C7).
- Forearm flexor weakness and intrinsic weakness (C8-T1).
- Rhomboid atrophy (dorsal scapular nerve C4-5).
- Winging scapula due to serratus anterior (long thoracic nerve C5-7).
Summary
BPI is a common injury in the contact sport athlete. It is usually caused by a traction of the brachial plexus due to a rapid contralateral side flexion of the neck with associated scapula depression. These tend to be the more benign grade 1 (neuropraxia) type lesions that recover spontaneously within 24 hours. The more severe grade 2+ injuries that may involve nerve rupture or avulsion are rare. In a follow-up to this article, we will discuss the investigations required to ascertain the severity of the injury and how these injuries are managed from conservative rehabilitation through to surgical repair of avulsed and/or ruptured nerves.References
- 2011. 13(4); 353-363
- 1979. 241 1480-1482, 1979
- J Shoulder and Elbow Surgery. 2014. 23. E293 e299
- 199321(5); 650-655
- J Bone Joint Surg. 1967. 49A 785-792
- 1965. 192 117
- The British Journal of Physical Medicine, Including Its Application to Industry. 1954. 17: 136–138
- Hand Clinics. 2005. 21: 13–24
- J Am Acad Orthop Surg. 2005;13(6):382-396
- 1943. 66: 238–288
- 1951. 74: 491–516
- Am J Sports Med. 1977. 5 209-216
- Clin Sports Med. 2002;21:29-35
- Millesi H (1991) Brachial Plexus Injuries. In: Jupiter JB (ed.) Flynn’s Hand Surgery, 4th ed. Baltimore, Md: Williams & Wilkins, 457–463
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.