Bridging the gap: from active to sports ready!

The goal of rehabilitation following a sports injury is to bridge the gap from an injured state to full sports readiness. This requires extensive planning to ensure loading produces the appropriate tissue adaptation to withstand the imminent sporting demands – but without causing re-injury.
Most athletes despair at being injured and urgently seek early reintegration to training and return to sport (RTS). The risks of re-injury following RTS vary among conditions and sports. However, for some of the common sports injuries, the statistics are alarmingly high. For example, evidence suggests that 30% of anterior cruciate ligament reconstructions will undergo a second surgery within 2 years of RTS(1).
Studies also show that younger athletes - aged 15-20 years – tend to return to sport earlier than those of adult age (21+ years) following an injury(1). This may be due to younger athletes having high levels of drive and low fear of re-injury, despite needing more time for neuromuscular and strength recovery compared to adults. Yet, they frequently return to higher volumes of training with greater demands(2).
Conversely, the athlete or clinician who progresses rehabilitation too cautiously risks a delayed RTS. This also presents complications such as fear avoidance, reduced confidence or psychological readiness, muscle inhibition, loss of skill, strength, and power. It is up to the clinician to set realistic expectations on RTS timeframes, and continuously adjust these to reflect the athlete’s condition and ability at each stage.
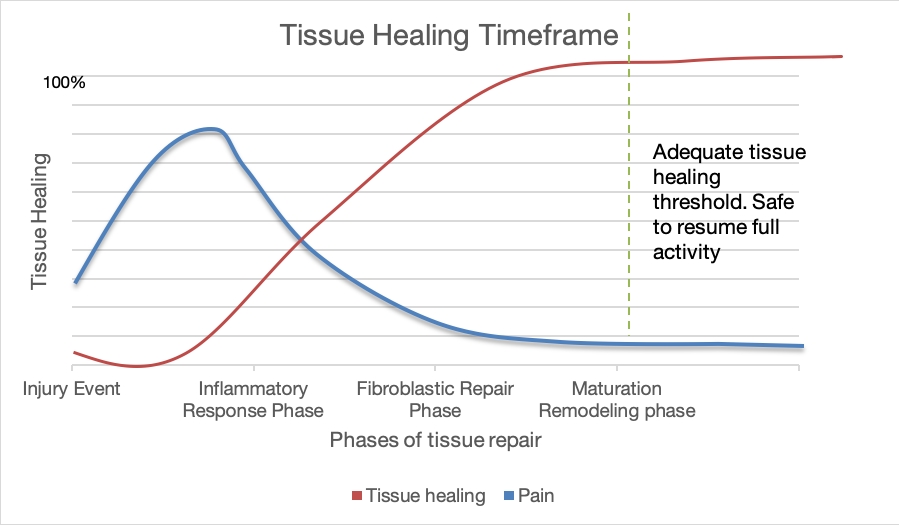
Achieving full muscle function is vital to successful rehabilitation and RTS. Rehabilitation should begin immediately following an injury and aim to develop re-activation of muscle activity, followed by strength, power, and endurance. Correct loading at each stage of healing creates positive tissue adaptation and on-going progression (see figure 1).
Figure 1: Tissue healing timeframe
Consequences of muscle injury
Following injury, a muscle can undergo rapid muscle atrophy due to the acute inflammation, response to pain, and immobilization. Even short periods of inactivity cause a reduction in strength, and endurance. These acute factors, along with pain, can weaken the neural input and prolong or worsen the strength deficits. Early muscle conditioning is therefore essential to minimize injury effects and the losses.Relative rest should commence immediately following muscle injury. This is to allow rapid and complete recovery. This rest period allows the connective tissue between the muscle injury sites to gain the strength required to withstand the forthcoming contraction forces without re-rupturing. Re-ruptures are the most severe muscle injury and often delay RTS(4). However, this rest period should be less than a week to ensure minimal scar tissue formation(5). Early mobilization with active exercise and loading is then encouraged to increase blood flow to the injury and accelerate the regeneration of the muscle fibers. Active exercises can be performed as isometric, concentric, or eccentric (see panel 1).
Panel 1: Exercise style definitions
Isometric: The muscle contracts but there is no movement associated with the contraction because the contractive and resistive forces are equal.Concentric: Muscle fibers shorten during the contraction because the contractile force is greater than the resistive force, so the muscle origin and insertion move towards each other.
Eccentric: Muscle fibers lengthen during the contraction because the contractile force is less than the resistive force, so the origin and insertion move further apart.
*Isometric contractions
Isometric exercises are often the starting point in a rehabilitation program. They allow loading to occur without movement, which is ideal when the injured limb is either immobilized, too painful to move, or too weak to contract. Performing isometric contractions early can prevent muscle atrophy by allowing static contractions and thus building static strength(6). The muscle contraction increases blood flow and aids reduction in swelling. As this is a static movement, any functional strength gained will be at the length it is performed; when pain allows, therefore, position the muscle at various lengths and perform isometric contractions along the entirety of the muscle.
Isometric exercises should be held for five seconds, with ten seconds of rest. They should be completed multiple times per day and performed in sets of ten(6). When these can be performed with maximal force and no pain, the athlete should progress to dynamic exercises in order to increase muscle loading. Initially, collagen fibers (which form the foundation of tissue repair) are aligned transversely to the injury site, which limits the force muscles can produce. Progressive loading shifts the type III collagen fibers to the stronger type I fibers and aligns them longitudinally along the line of stress. This fiber alignment greatly improves strength and function(7). Load an injury too lightly, however, and the newly formed fibers will not align optimally and could also form scar tissue adhesions, hindering future function.
*Concentric/eccentric contractions
Concentric and eccentric muscle contractions provide different stimuli to a muscle and therefore result in different muscle adaptations(3). Eccentric loading can develop greater forces in a muscle compared to concentric loading. As strength gains are proportional to the size of force developed, eccentric exercises are therefore capable of producing greater total strength, muscle mass, and muscle cross-sectional area(1-3). The increased loading that occurs with eccentric exercises causes certain changes that are not observed after concentric loading. In particular, eccentric contractions:
- Lengthen the muscle-tendon unit, therefore reducing the strain on the tendon during activity(8).
- Change the metabolism of the muscle/tendon and alter pain perception, allowing further loading without pain(8).
- Stimulate the synthesis of type I collagen fibers (the stronger fibers)(9).
- Allow greater forces to be applied, thereby causing an increased remodeling stimulus(8).
- Cause a fluctuation of repeated loading and unloading during the contraction, which gives a fluctuation in force-induced, and therefore a greater remodeling stimulus(10).
Eccentric exercises might appear to be the optimum loading strategy to produce enhanced strength benefits as described above. However, eccentric loading strength gains are most effective at producing greater eccentric strength; concentric exercises are needed to guarantee gains in concentric strength too. Eccentric exercises also produce greater transient muscle damage, muscle soreness, and force impairments, so they must be used in the correct situation under controlled conditions in order to ensure progression rather than regression(11).
Loading principles
Following isometric exercises, muscle loading principles should begin with low load, high-repetition exercise to allow muscle activity stimulation and muscle patterns to form. Initial strength gains are due to an increase in neural adaptations (ie the brain’s input is strengthened from the muscle activity and it learns how to produce more force from the contracting muscle)(12). To progress strength enough to withstand the required forces, and to produce hypertrophy, muscle overload should occur with applying increased loads. Eventually, power development should be incorporated in order to replicate forces produced in sport. Power is progressed by increasing speed of muscle contractions, functional exercises (such as jump squats or bounding), and by the introduction of plyometric exercises (see table1).| Exercise principle | Definition | Suggested format |
|---|---|---|
| Strength | The ability to exert force | Increase load and increase repetitions |
| Power | The rate of work performed by muscles “ calculated by the product of the force exerted and the distance moved(7) | Increase speed of resistance exercises |
| Endurance | The muscles ability to sustain contraction or perform repeated contractions(6) | Increase volume with low load and high repetitions |
Rehabilitation example
Here is a proposed example for progressing a knee injury such as a patellar dislocation/patellar tendon/quadriceps strain, from the initial injury through to end-stage loading (see table 2).| Timescale for injury | Suggested stage of healing | Type of loading | Load amount | Exercise suggestions |
|---|---|---|---|---|
| 0-72 hours | Acute inflammatory stage | Rest | Nil | Hip abductions, hip rotation exercises, heel raises; to protect the knee joint, while maintaining musculature at the joints above and below |
| 2 days up to 4-6 weeks | Proliferation/repair stage | Isometric then progress to concentric/eccentric as appropriate | Under 50% 1RM | Static quadriceps contractions, progressing to various angles, eg straight leg raise, knee extensions |
| 4 weeks to 3 months | Remodeling/maturation stage | Concentric/eccentric | 50-75% 1RM | Single leg squat off a step, squats on a decline board |
| 6 weeks to12+ months | Remodeling/maturation stage | Concentric/eccentric | Greater than 75% 1RM | Squats, lunges, multi-direction lunges with speed, running drills, hops & bounds |
Summary of the key points
- Athletes who return to sport prematurely increase their risk of re-injury. However, if rehab is not progressed adequately, the risk of fear-avoidance, reduced strength and delayed motor patterns increases.
- Full muscle conditioning requires an initial period of rest followed by progressive muscle loading in the forms of isometric, concentric, and eccentric exercises. All types should be prescribed, but their quantity and time of use will vary.
- Isometric exercises are predominantly used first to load the injury almost immediately. Following on with eccentric exercises allows higher force production and greater strength gains, but has associated risks and should, therefore, be prescribed accordingly.
- End-stage rehabilitation should mimic the loads sustained in the athlete’s sport in terms of quantity, speed, and time under load.
References
- Knee Surg Sports Traumatol Arthrosc. 2018. 26;1966–1974
- Br J Sports Med. 2018. Dec:52(23); 1482-1483
- Frontiers in Physiol. 2017. Jul:8(447); 1-16
- Am j Sports Med. 2006. 34: 1297-1306
- Muscle, ligament & tendon J. 2013. 3(4): 337-345
- Clinical Sports Medicine.2009. 3E Rev. McGraw-Hill Professional
- Essentials of Strength Training and Conditioning. 4E. Human Kinetics
- Br J Sports Med. 2009. 43: 556-568
- J Orthopaedic S Phys Therap. 2015. Nov: 45(11); 853-863
- Br J Sports Med. 2009. 43: 242-246
- Sports Med. 2004. 34: 49-69
- Am J Phys Med. 1979. 58: 115-130
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










