Getting to grips with the distal radioulnar joint

Anatomy and Biomechanics
The distal radioulnar joint (DRUJ) allows pronation and supination of the forearm. Along with the proximal radioulnar joint (PRUJ), these two uniaxial pivot joints simultaneously create forearm pronation and supination. Most of the movement originates in the PRUJ as the radius rotates around the ulna, but the DRUJ allows a degree of freedom at the ulnar head(2). Incidentally, the forearm has greater supination with 90 degrees of elbow flexion and greater pronation in full elbow extension(3,4).- Articular skeletal structure
The arrangement of the DRUJ involves the sigmoid notch of the radius and the ulnar head. This skeletal arrangement provides minimal stability as the sigmoid notch is shallow and radius curvature is 50% greater than the ulnar head(5). There are four sigmoid configurations within the DRUJ with varying degrees of stability at each articulation (see figure 1)(6).
Figure 1: Anatomy of the distal radioulnar joint
Adapted from The Open Orthopedics Journal, 2012, 6, 204-210 and used under the Open-Access License.
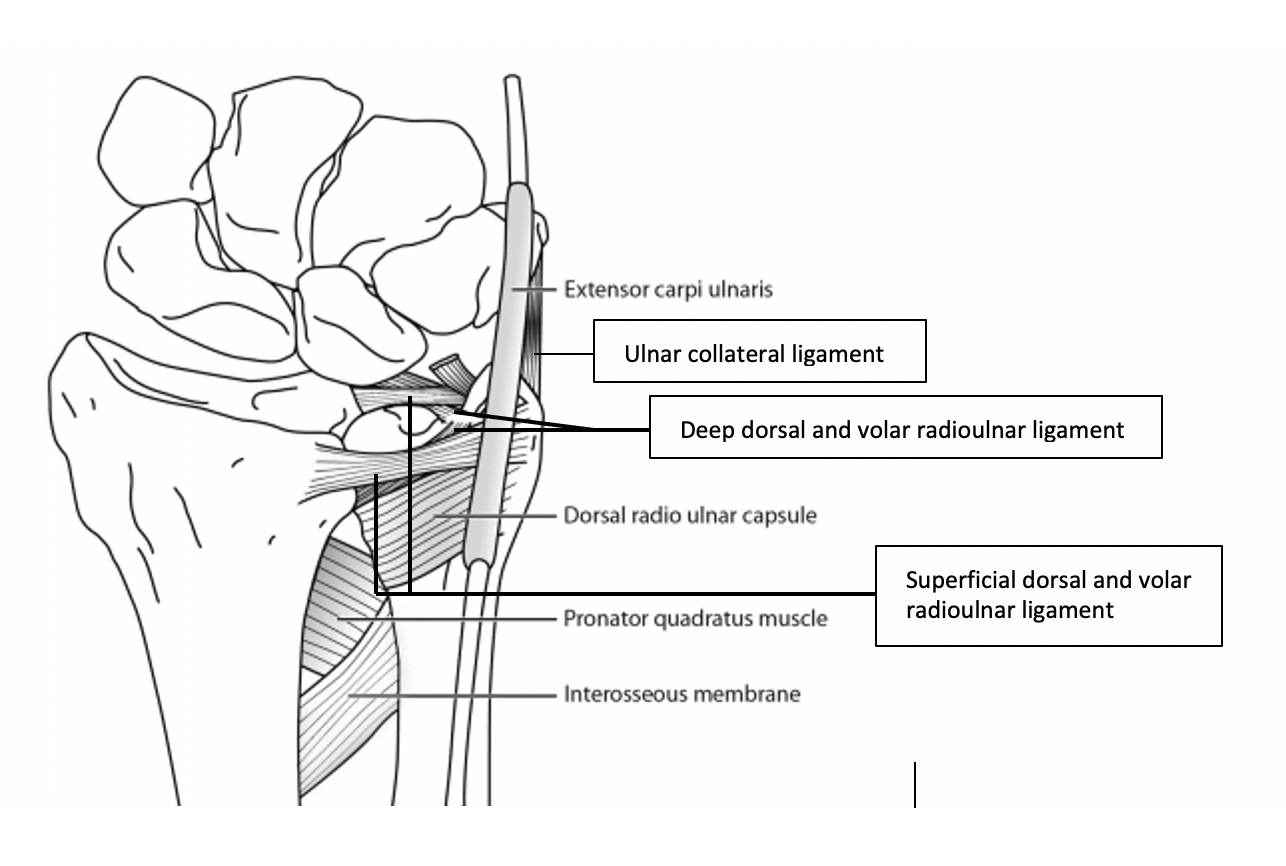
- Triangular fibrocartilage complex (TFCC)
The TFCC comprises of five distinct parts: an articular disc, the deep dorsal and volar radioulnar ligament, the superficial dorsal and volar radioulnar ligament, and two disc-carpal ligaments(8). The volar and dorsal radioulnar ligaments work agonistically during pronation and supination to allow a smooth transition during rotation(7,9,10). Disruption of the volar and dorsal radioulnar ligaments leads to gross instability of the DRUJ (see figure 2)(11).
Figure 2: The relationship between the volar and dorsal radioulnar ligaments
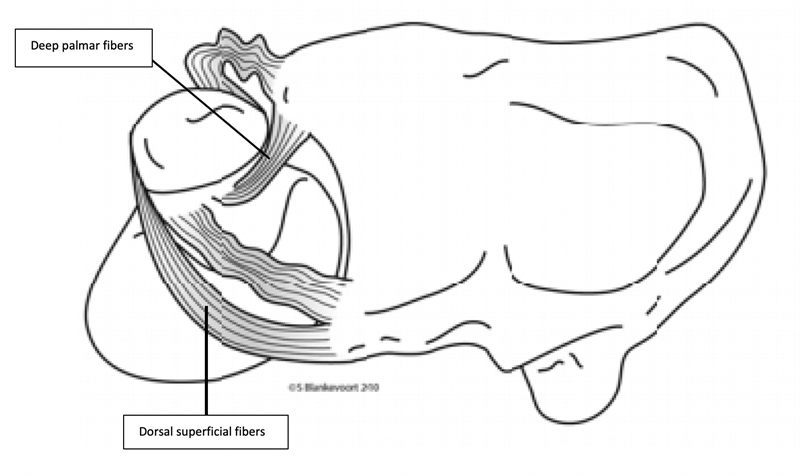
In pronation, the superficial dorsal and deep palmer fibers tighten to keep the DRUJ stable. In supination, the superficial palmer fibers and the deep dorsal fibers both tighten to provide stability. Adapted from The Open Orthopedics Journal, 2012, 6, 204-210 and used under the Open-Access License.
- Extensor carpi ulnaris (ECU) tendon
The location of the ECU is on the dorsomedial side of the forearm. The tendon attaches to the ulnar head via the fibro-osseous tunnel and then inserts on the base of the 5th metacarpal(12). Thus, the ECU functions as a dynamic stabilizer during forearm supination.
- Pronator Quadratus Muscle (PQM)
The PQM comprises two distinct heads: the superficial head, which originates on the dorsal border of the ulna and inserts onto the palmar surface of the radius, and the deep head, which originates on the ulna and inserts onto the ulnar side of the distal radius(13). The deep head extends to the interosseous membrane and covers the DRUJ capsule(14). The PMQ is the primary pronator of the forearm and provides dynamic stability to the DRUJ during pronation and supination(14,15).
- The interosseous membrane (IOM)
The IOM runs obliquely from the distal ulna to the proximal radius, and the central band is known as the interosseous ligament (IOL). This ligament has mechanical properties like the patellar tendon and stiffness similar to the ACL. The IOL resists proximal translation of the radius(16).
Mechanism of injury and presentation
The mechanisms of injury commonly associated with DRUJ injuries are a fall onto an outstretched hand (FOOSH), an unexpected forceful rotation of the forearm, direct trauma, or axial distraction of the wrist(6,17,18). In addition, an avulsion of the DRUJ volar ligament leads to a subluxation of the ulnar head. These injuries are associated with forced or repeated pronation during contact or wrist loading sports such as gymnastics(19).- Distal radial fractures
There is a range of different fracture possibilities that involve the DRUJ. Fractures that disrupt the joint include sigmoid notch, ulnar articular, styloid process, and forearm fractures. The outcome of these fracture types may cause radial shortening or angulation(20).
- TFCC injuries
Injuries to the TFCC may be traumatic or degenerative.
- Instability/dislocation of the DRUJ
As with other joints, the DRUJ may be subject to both traumatic dislocation and subtle instability. Dislocations may occur with significant injuries to the TFCC and associated fractures of the sigmoid notch and ulnar head. The common mechanism of injury is hyper-rotation or a direct blow(21). Subtle DRUJ instability may present with ulnocarpal pain, clicking with rotation, pain in loaded positions, and swelling on the ulnar side. Dorsal dislocations are more common than volar and usually occur during forced pronation movements. The injury leads to limited supination and a dorsal ulnar head prominence. Conversely, volar dislocations occur during forced supination and result in limited pronation(17).
Frank dislocations are obvious; however, on initial examination, clinicians may miss a subtle DRUJ instability. Imaging will provide reliable diagnostic criteria for DRUJ and TFCC injuries(22).
- Dorsal Displacement of Radius
High force overpronation injuries or direct blows to the radius may cause a dorsal displacement. This mechanism may cause injuries to the ECU subsheath, the dorsoulnar portion of the TFCC, the ulnar collateral ligament, the joint capsule, and the proximal attachment of the TFCC(23).
- Subluxation related ulnar neuropathy
A DRUJ instability may kink the ulnar nerve as it passes through the fibro-osseous ulnar canal at the wrist. A distortion of the nerve may lead to transient neurological deficits in its motor and sensory distribution. Supination aggravates the symptoms, and electrodiagnostic testing is usually negative(22).
Physical examination
There are several tests available to assess and diagnose DRUJ Instability (see table 1). These tests have varying degrees of reliability. Due to the complex anatomical nature of the wrist, the tests are best used collectively and related to the patient's clinical presentation.| Name | How to perform | Positive if: | Tested stabilizer | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|
| Stress test/ballottement/ œpiano sign | Elbow flexion 90 degrees, fingers to the ceiling. Dorsopalmer movement of the ulna in respect to the radius in maximal pronation and supination | Painful or DRUJ laxity | Palmer and dorsal ligament subcruentum | 0.66% | 0.68% |
| Radius pull test | Elbow flexion 90 degrees with wrist in neutral position, pulling the radius in longitudinal direction | Ulnar variance increases during pulling under fluoroscopy | Interosseous membrane | Up to 100% in cadaveric studies | Up to 100% in cadaveric studies |
| Clunk test | Compress ulna to the radius during passive pronosupination | A clunk is palpable for the patient | Interosseous membrane | Not available | Not available |
| ECU test | Elbow flexion 90 degrees, hand in ulnar deviation, active pronosupination | Abnormal motion ECU tendon | ECU tendon | Not available | Not available |
| Press test | Patient pushes up from a seated position with the use of affected wrist | Focal ulnar sided wrist pain | TFCC | 100% | Not available |
Radiological imaging
The four most reliable imaging features suggestive of DRUJ and TFCC injury are basal fracture of the styloid of the ulna, widening of the DRUJ joint space, dislocation of the radius relative to the ulna on the lateral view, and greater than 5mm shortening of the radius(23).- X-ray
Plain anterior-posterior (AP) and lateral views will demonstrate significant distal radius and ulnar head fractures. However, they may miss subtle DRUJ instability due to the overlap of the radius and ulna on lateral views. Therefore, if a DRUJ instability is suspected, loaded views are needed to see the displacement(26).
- Computerized Tomography (CT)
Computerized Tomography may show subtle displacement of the DRUJ, minor fractures, and abnormalities of the sigmoid notch. These should be performed in neutral or in positions of maximal pain to view structural pathologies(27).
- Magnetic Resonance Imaging (MRI)
An MRI will allow visualization of the entire TFCC soft tissue complex. It has a sensitivity of 100% and specificity of 93% in detecting TFCC tears(28). An MRI can diagnose ulnar impaction syndrome, perforation of the lunotriquetral ligament, subchondral sclerosis, and articular cartilage defects in the ulnar head and associated carpal bones(29).
Management
The management of DRUJ injuries is dependent on the type and severity. The conservative management of mild injuries includes splint bracing, while more serious damage requires either non-operative or operative reduction. Frank dorsal dislocations may be manually reduced with direct pressure on the distal ulna while undergoing forceful supination. Clinicians may reduce volar dislocations with pressure on the volar side and forced pronation. The reduction is immobilized in a below shoulder cast for six weeks to prevent any elbow motion.Indications for surgical management include cases where there is soft tissue interposition that prevents conservative reduction, a locked DRUJ, sigmoid fractures that lead to instability, and chronic instability. Distal radius or ulnar head fractures also require correction. Malunion of these distal segments will lead to instability and incongruity of the DRUJ, thus placing stress on the TFCC complex(26). The surgical technique selected will depend on the type and severity of the DRUJ injury and the involvement of the TFCC(29). Osseous avulsions of the TFCC may undergo refixation surgery. Tears of the superficial TFCC require simple arthroscopic fixation, whereas deep tears require anatomic transosseous refixation. Complete TFCC tears require open anatomic refixation, and unrepairable injuries require a tendon graft reconstruction(30).
Conclusion
The assessment and diagnosis of DRUJ injuries are daunting and difficult during the acute examination. Functional deficits such as loss of grip strength, pain on full pronation and supination movements, and an inability to load through the wrist should be key clinical indicators for the presence of DRUJ instability. Sound anatomical and biomechanical knowledge will assist clinicians in accurately diagnosing, investigating, and managing DRUJ injuries. The correct management of these injuries is vital to ensure that athletes return to sport without chronic instability and reach their pre-injury performance level.References
- Am J Sports Med. 2003; 31(6), 1038-1048
- Handchir Mikrochir Plast Chir. 1994. 26; 22-26.
- J Hand Surg Eur Vol 2008; 33: 3–8
- Ann R Coll Surg Engl 2013; 95: 163–170
- Scand J Plast Reconstr Surg 1985;19: 17-25.
- The Journal of Hand Surgery. 2017. 42E(4), 338-345.
- J Hand Surg Br 1996; 21: 581–586.
- Clin Orthop Relat Res. 1989. 245: 123-32.
- J Hand Surg Am 2007; 32: 1,086–1,106.
- J Hand Surg Am 2009; 34: 40–45.
- J Hand Surg [Am] 1995; 20:930-936
- Clin Orthop. 1970. 68:124-9.
- J Hand Surg Am. 2001. 26(6); 1129-34.
- J Orthop Res. 2004, 22: 208-13
- J Hand Surgery Br. 1996, 21: 581-6.
- J Hand Surg Am. 1997, 22. 981-5.
- J Hand Ther. 1996. 9:129-38.
- J Hand Surg Am. 2012. 37; 1489-1500.
- Brukner P. and Khan. K. (2017) Clinical Sports Medicine. Vol 1. 5th McGraw Hill. Australia.
- J Hand Surg [Br]. 1998. 23B:507-511.
- Hand Surg. 2013; 18(1). 21-6.
- Clin Orthop. 1985. 194:189-94.
- 2012. 43: 926-32
- J Hand Surg Eur Vol. 2011 Dec 22.
- Open Orthop J. 2012. 6: 204-210.
- Hand Clin.1991. 7:311- 27.
- Skeletal Radiology. 2016. 45(11), 1487-93
- 1989. 173; 723-729
- Steinbach LS, Smith DK (2000): MRI of the wrist. Clinical Imaging 24:298-322. Stewart NR, Gilula LA (1992): CT of the wrist: a tailored approach. Radiology. 183:13-20.
- Archives of Orthopaedic and Trauma Surgery. 2020. 140; 639-650.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









