Long COVID: returning athletes from the deep

Soon after the pandemic, recovered patients began complaining of complications beyond the initial acute infection period. The incidence of Long COVID is high, with 25% of individuals reporting symptoms for more than one month and 10% experience symptoms beyond 12 weeks(1).
Definition
The NICE guidelines define Long COVID as continuous and prolonged symptoms beyond one to three months post-acute viral infection(2). To diagnose an athlete with Long COVID, the clinician should ensure the symptoms are not a result of an unrelated infection or medical condition. It may be difficult to distinguish from common seasonal infections, and thus a thorough medical assessment is advised.Signs and Symptoms
The symptoms associated with Long COVID may be systemic and adapt over time (see table 1). However, the most common symptoms described by individuals are fatigue and dyspnoea(3).Table 1: Multi-systemic symptoms associated with Long COVID(2).
| System | Symptoms |
|---|---|
| Respiratory | Breathlessness |
| Cough | |
| Cardiovascular | Chest tightness |
| Chest pain | |
| Palpitations | |
| Generalized | Fatigue |
| Fever | |
| Pain | |
| Neurological | Cognitive impairment |
| Headache | |
| Sleep disturbance | |
| Peripheral | |
| Neuropathy | |
| Dizziness | |
| Delirium | |
| Gastrointestinal | Abdominal pain |
| Nausea | |
| Diarrhea | |
| Anorexia | |
| Musculoskeletal | Joint pain |
| Muscle pain | |
| Psychological | Depression |
| Anxiety | |
| Ear/nose/throat | Tinnitus |
| Earache | |
| Sore throat | |
| Dizziness | |
| Loss of taste/smell | |
| Dermatological | Skin rashes |
Pathophysiology
The pathophysiology of Long COVID is currently unknown. The severity of the disease does not influence the risk of developing Long COVID, as mild infections could have persistent effects. However, several different mechanisms are likely responsible, owing to the spread of diverse symptomatology, and currently, two theoretical models exist.1. Unresolved inflammation
The SARS-COV-2 virus binds to receptors found in the lungs, heart, liver, kidneys, and blood vessels(4). One cause of inflammation may be systemic viral persistence as viral shedding in the respiratory tract is possible for up to four months post-infection(5). Viral shedding is also possible in feces, indicating multi-organ involvement(6).
In addition, a COVID-19 infection may result in B and T cell lymphocyte deficiency which may increase the time taken to resolve inflammation post-infection. The viral persistence and suppressed immune response may lead to unresolved inflammation and contribute to the symptoms and duration of Long COVID(7,8).
2. Long-term tissue damage
The possibility of multi-organ involvement is high due to viral dissemination. In addition, tissue fibrosis has been demonstrated four months after acute infection, with the lungs and heart at particular risk(9). For example, researchers at The First Affiliated Hospital of Zhengzhou University in China found pulmonary changes and abnormalities on MRI in 71% of cases three months after an acute infection, and 25% of participants had functional impairments(10). In some cases, CT chest radiography demonstrates long-term lung fibrosis six months post-COVID infection(11).
Metabolic abnormalities and structural brain changes may explain the neurological complications associated with Long COVID. The brainstem has higher quantities of receptors with an affinity to SARS-COV-2 than other brain regions(12). This may lead to neurological and cardiorespiratory dysfunction(13). In addition, researchers at University Hospital Frankfurt in Germany found cardiac abnormalities and myocardial inflammation on MRI on individuals with persistent symptoms(14).
Assessment and management
Due to the complexity of Long COVID, a multi-disciplinary approach is most beneficial. There is no specific diagnostic test, and the prognosis is challenging. Therefore, a patient-centered approach is advantageous(4). The World Health Organization recommends that rehabilitation includes education on the conservative resumption of daily activities and submaximal pacing that is safe and manageable(1). To best guide the management, four groups have been identified (see table 2).Table 2: A summary of the classification, assessment, and management of Long COVID(1).
| Classification | Description | Symptoms | Assessment | Management |
|---|---|---|---|---|
| Post-exertional symptom exacerbation | The experience of fatigue or exhaustion that results from previously tolerated activity. | Fatigue and exhaustion | Self-report questionnaire | Pacing |
| Cognitive dysfunction | Two-day cardiopulmonary exercise testing (CPET) | Heart rate monitoring | ||
| Pain | Six-minute walk test | |||
| Fever | Activity monitors | |||
| Sleep-disturbance | ||||
| Diarrhea | ||||
| Exercise intolerance | ||||
| Cardiac impairment | Exacerbation of cardiac-related symptoms on the resumption of physical activity. | Tachycardia | Physical Activity Readiness Questionnaire for Everyone | Referral to cardiologist |
| Chest Pain | Physical Activity Readiness Medical Questionnaire | Echocardiogram (ECG) | ||
| Dyspnoea | Holter monitor | |||
| Hypoxia | Echocardiography | |||
| Palpitations | Cardiac MRI | |||
| Exercise intolerance | ||||
| Exertional oxygen desaturation | A fall of >3% in oxygen saturation during or after mild exertion. | Hyperventilation | Pulse-oximetry monitor | Saturation monitoring |
| Increased tidal volume on exertion | The monitoring of oxygen saturation on a 40-step walk and the one-minute sit-stand test | Pacing | ||
| Oxygen desaturation >3% | ||||
| Chest pain | ||||
| Fatigue | ||||
| Dizziness | ||||
| Syncope (fainting) | ||||
| Autonomic nervous system dysfunction | A change in the autonomic nervous system that affects health. | Postural orthostatic tachycardia syndrome (POTS) | NASA-10-minute lean test | Pacing |
| Orthostatic intolerance | Active stand test | Autonomic conditioning therapy (Breathwork, supine exercises, symptom titrated submaximal aerobic exercise) | ||
| Breathlessness | COMPASS 31 score | |||
| Fatigue | Heart rate variability, heart rate recovery, and heart rate acceleration | |||
| Pre-syncope (feeling faint) | ||||
| Palpitations | It is essential to exclude myocarditis, pneumonia, or pulmonary embolism. |
________________________________________________________________________________
What is pacing?
Pacing is an approach to managing activity levels with rest to avoid worsening symptoms. Pacing includes identifying realistic goals, monitoring physical, cognitive, and social activities and their effects on energy levels, and avoiding over-exertion(1). An empathetic therapeutic relationship is vital to facilitate the engagement of the athlete in the rehabilitation process. Practitioners need to be receptive and include an athlete’s beliefs and experiences into the rehabilitation care plan. To stabilize symptoms, a holistic approach, which includes rest, sleep management, and appropriate nutrition, is key to rehabilitation success(1). Valuable resources on pacing are available from the Long COVID Physio website.
________________________________________________________________________________
Before starting rehabilitation, in persistent symptoms, the first step is to rule out other medical conditions. For example, individuals recovering from an acute COVID infection are at increased risk of developing new cardiovascular and respiratory diseases(15). The screening and assessment of an athlete before return to activity will assist in avoiding a ‘relapse’ and worsening of symptoms. It will also provide the clinician and athlete with a framework to develop realistic goals and care plans. While validated initially for use in chronic fatigue syndrome, the DePaul Symptom Questionnaire covers many chronic symptoms and provides practitioners with an easy-to-use assessment tool (see figure 1)(16).
Practitioners need to continuously monitor and adjust physical activity according to symptoms(17). While graded exercise return has been a cornerstone for other rehabilitation, it is not recommended for chronic fatigue, similarly for Long COVID(18). Instead, practitioners should advise strategies to control and limit the symptoms, adequate pacing, and teach flexibility to allow schedule changes and activity modification. An adaptable, not a graded, approach should allow pacing without pushing through symptoms and rest when appropriate. Due to the risk of worsening symptoms, practitioners should apply interventions with caution, and the aim should be sustainable symptom stabilization to improve daily functioning over time.
Figure 1: A Brief Questionnaire to Screen for Post-Exertional Symptom Exacerbation(19).
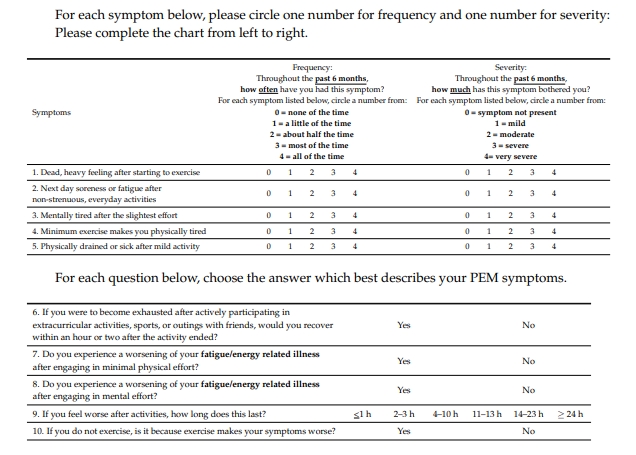
A score of 2 on both frequency and severity on any items 1 to 5 indicates post-exercise malaise. The five supplemental questions are also available to examine and monitor the duration, recovery, and exercise exacerbation.
Conclusion
Long COVID is a new and complex condition that requires the attention of public health and sports medicine practitioners globally. As further evidence emerges, the management of Long COVID is likely to improve, but we need to provide athletes with authentic care options until then. One of the keys to successful management is recognizing the signs and symptoms and ensuring that it is safe to proceed. The safe implementation of physical activity interventions requires informed clinical decision-making, carefully planned rehabilitation strategies, and constant symptom monitoring.References
- World Physiotherapy Briefing Paper 9, 2021
- NICE Guideline Post-Covid, 2020
- BMJ. 2021;372:n136
- The Lancet. 2020; (386):1861
- Emerg Microbes Infect. 2020; 9(1):2571-2577.
- Clin Gastroenterol Hepatol. 2021; 19(7):1387-1394.e2.
- Infect Dis. 2021: 1–18
- Immunol Lett. 2020; 225:31-32.
- BMJ Open 2021;11:e048391
- EClinicalMedicine. 2020;25:100463
- Radiology. 2021;299(1): E177–E186.
- EClinicalMedicine. 2020;25:100484
- ACS Chem Neurosci. 2021; 12(4):573-580.
- JAMA Cardiol. 2020; 5(11):1265-1273
- BMJ. 2021;372:n693
- 2019;7(3):166-179.
- NIHR Themed Review: Living with Covid19 - Second review. 2021.
- BMJ2020;370:m2933
- Diagnostics2018, 8(3), 66
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.