Navigating sports medicine’s ‘Bermuda Triangle’ - part II

Athletic groin pain (AGP) is common among athletes participating in soccer, Australian rules football, Gaelic football, ice hockey, and rugby union(1,2). Traditionally, practitioners consider AGP as the ‘Bermuda Triangle’ of sports medicine, and part one of the AGP series provides guidelines regarding the assessment and diagnosis. Part two outlines the treatment and rehabilitation of AGP in the context of the control-chaos continuum(2,3,4).
Depending on the cause and severity, sports medicine professionals manage AGP with or without surgery and rehabilitation. Although surgery is unavoidable in specific circumstances, rehabilitation has significantly quicker return-to-play (RTP) rates, especially for abdominal and adductor-related AGP(5).
While AGP symptoms could initially be mild, resulting in occasional training absences, they could develop into career-altering disability or recurring injury if not appropriately managed. Like anterior cruciate ligament (ACL) and hamstring injuries, previous injury is a primary risk factor for athletic groin injuries(6). Considering the high re-injury rates, practitioners should reconsider if recurring groin injuries are unavoidable due to the nature of the sport or reflect the rehabilitation process’s failure to prepare athletes for the risks and demands of their sport.
Surgical intervention
Five gross etiologies may lead to groin pain requiring surgery: femoroacetabular impingement (FAI) (32%), athletic pubalgia (24%), adductor-related pathology (12%), inguinal-related pathology (10%), and labral pathology(1). Furthermore, hip arthroscopy is the primary treatment for FAI and labral pathology(1,5). Typically, surgeons will repair a sports hernia with open surgical procedures with or without mesh reinforcement while using open or laparoscopic repair techniques to treat inguinal pathology. Finally, the surgical treatment of adductor-related pathology is complete adductor tenotomy or reattachment procedures(1,5).Conservative treatment
Practitioners approach conservative AGP management with massage, mobilization, electrotherapy, and exercise interventions(2,7,8). Compared to passive physical therapy modalities, an active approach to rehabilitation, including supervised physical training, results in a higher successful RTP(2,8,9). Regardless of the classification of AGP, practitioners should direct exercise therapy to deficits identified during the physical assessment. Unfortunately, there is limited high-quality evidence for specific exercise interventions for the treatment and prevention of AGP. Poor research methodology, especially concerning the use of external load and progression methods, limits the quality of available evidence(10).Merging RTP frameworks
Return to play can be a long and challenging journey following complex sports injuries, such as AGP. Assessing the level of risk, planning, and adapting the RTP process involves merging high-quality evidence and practitioner experience(4,11). The RTP continuum and control-chaos continuum (CCC) provide practitioners with a progressive approach to planning and periodizing rehabilitation that allows athletes to return to pre-injury or improved performance levels(4,12).The RTP continuum emphasizes that the role of sports rehabilitation professionals stretches far beyond getting the athlete symptom-free and functional(12). This continuum defines three progressive stages: return-to-participation, return-to-sport, and return-to-performance. The CCC progress through five stages: high control, moderate control, control>chaos, moderate chaos, and high chaos(11). The CCC acknowledges that while rehabilitation occurs in a safe, structured, and controlled environment, the sports field can be unstructured and unpredictable. Principles of both these continuums require practitioners to understand the initial return-to-participation rehabilitation principles and the sport science-related physiological demands of athletes’ sports.
Meeting the demands of the sport
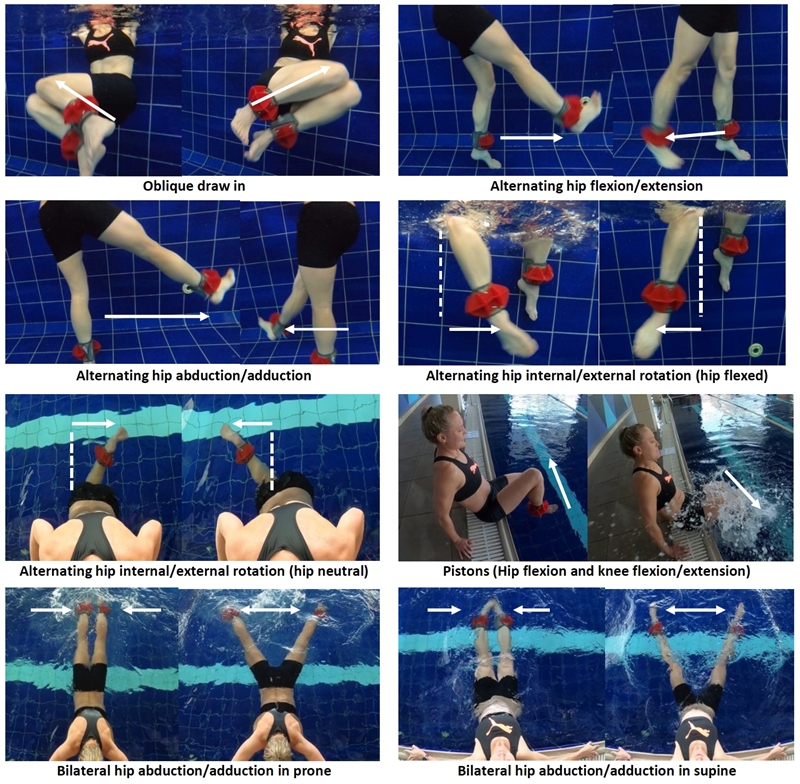
Dynamic correspondence refers to the ability of a training program to influence athletes’ performance(13). Similarly, methods employed in the initial phases of rehabilitation should prepare injured athletes for subsequent stages and ultimately optimal sports performance. Throughout rehabilitation, practitioners should consider the integrity of the injured structure and the risks and demands of the players’ sport, position, and level of play.The return-to-participation phase allows restoration of injured tissue integrity and builds athletes’ confidence to move(4). Following groin injuries, the rehabilitation focuses on synergistic training of the posterior and anterior myofascial chains, cardiovascular exercises, structure-specific exercises, general athletic capacity, and sport-specific training(6,14). Furthermore, interventions should simultaneously target the hip and trunk musculature(2,10). For example, aqua-kinetic-based exercises can simultaneously address all the above focus areas and allow practitioners to adapt the velocity, range, and frequency as tolerated by the athlete (see figure 1).
Figure 1: Aqua-kinetic exercises for strengthening of muscles of the hips and trunk
The CCC approach progressively re-introduces more game-like activities through five stages of rehabilitation(4). During the high and moderate control phases, practitioners introduce low-intensity straight-line and change of direction (COD). However, practitioners should ensure that athletes have the appropriate neuromuscular and power foundations before starting sport-specific exercises. For example, ball exercises that simultaneously challenge trunk, hip, and groin muscles can simulate athletic movements to develop foundational motor competency (see figure 2). In addition, exercises should activate the myofascial chains sufficiently similar to that of the activities involved in the athlete’s sport(13). Athletes can perform rehabilitation exercises slowly and in pain-free ranges in acute rehabilitation phases. After that, practitioners can increase the range and speed of movement, thereby eliciting and retraining the stretch-reflex(13).
Figure 2: Ball exercises challenging trunk, hip, and groin muscles and simulates athletic movements.
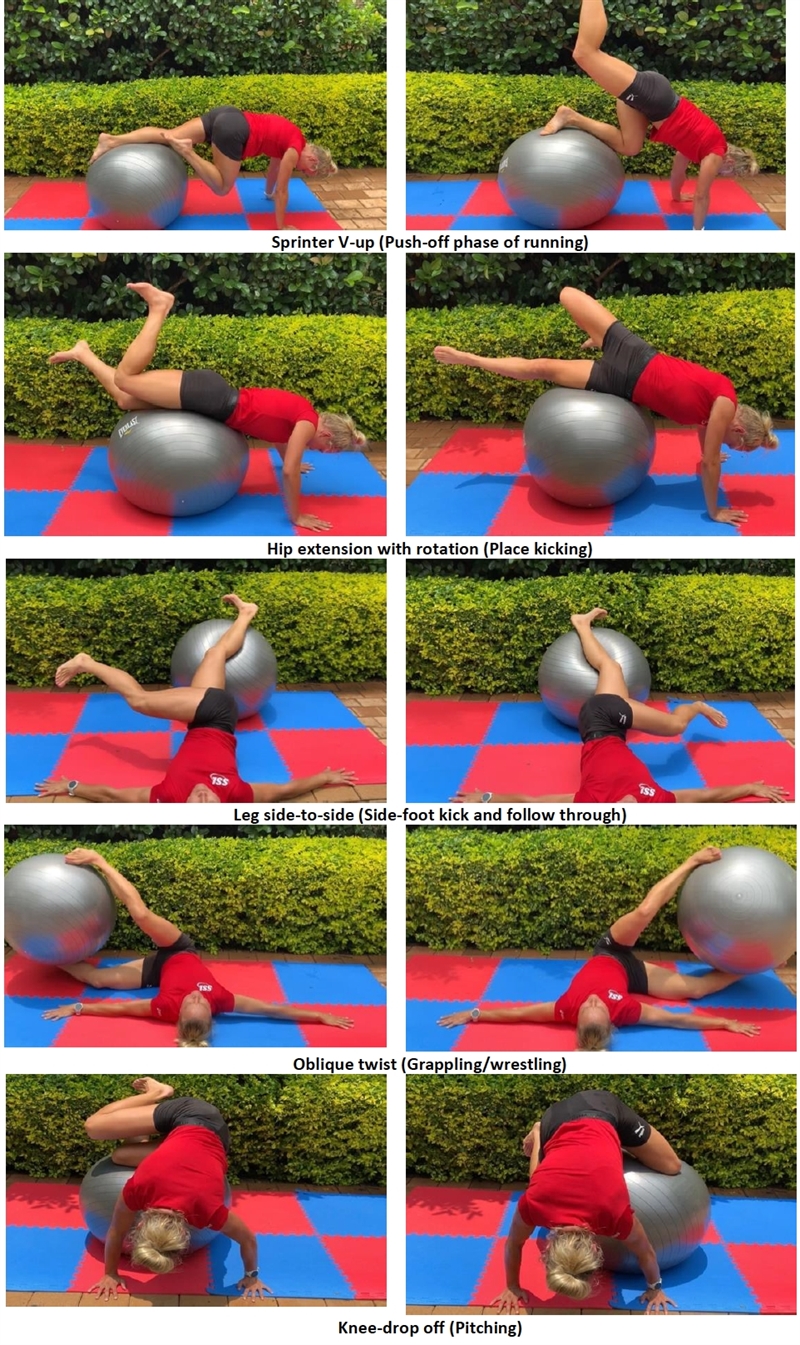
Figure 3: Multidirectional movement drills
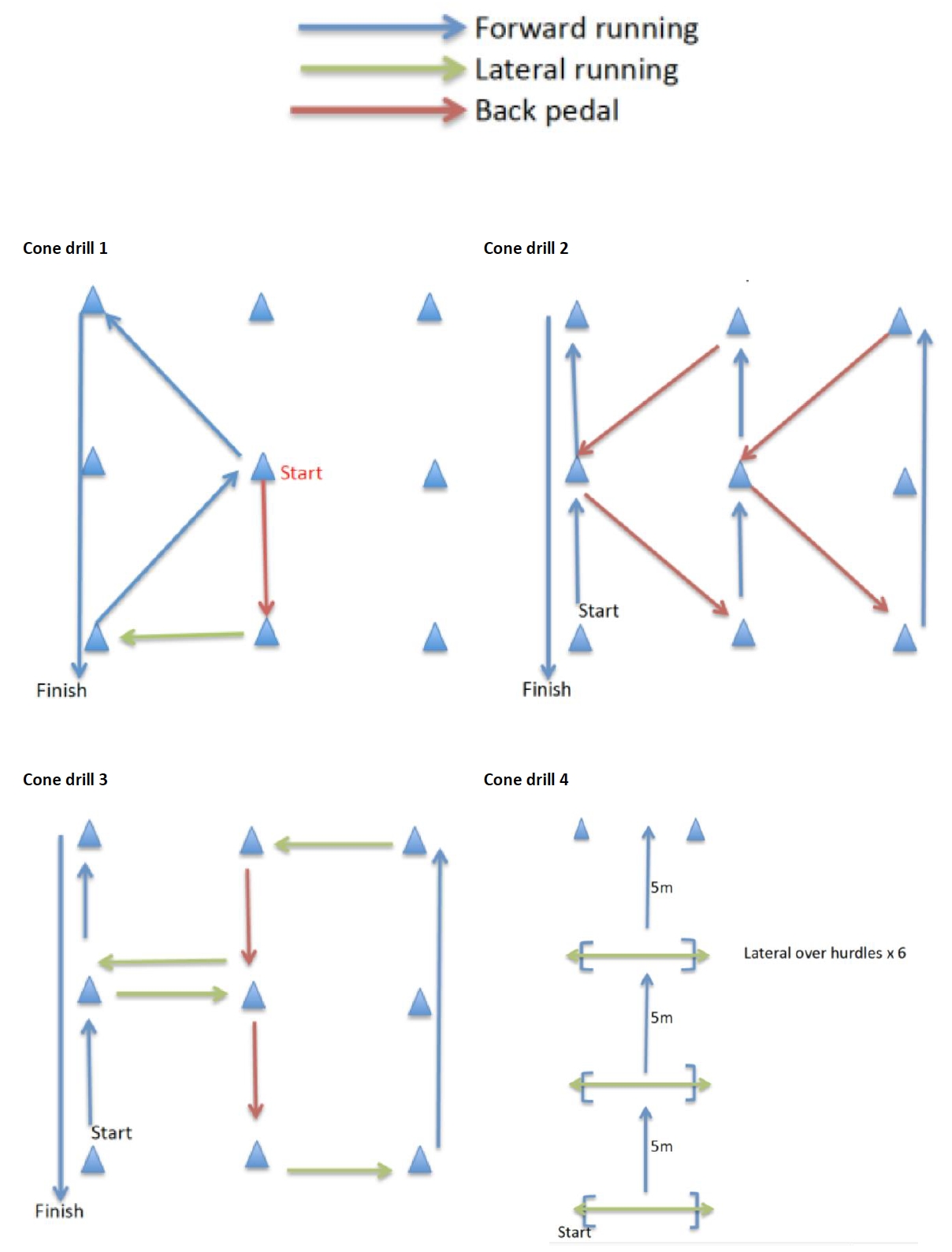
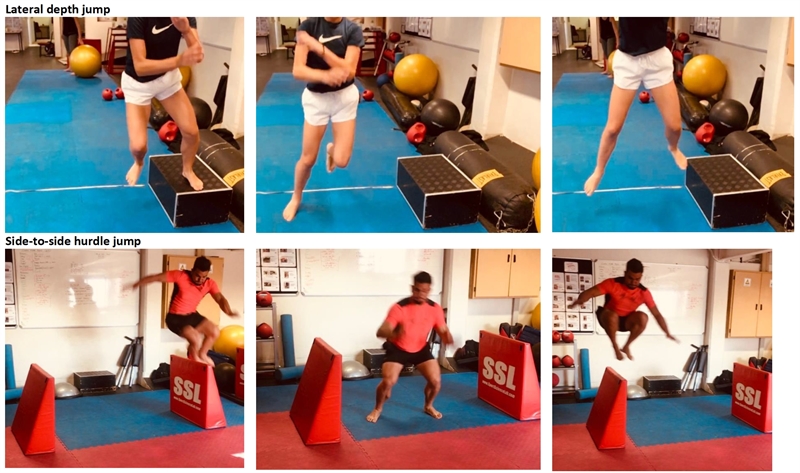
Rehabilitation drills are a cornerstone of the CCC, and sport specificity is vital to maintain player interest and develop confidence(11). During the high control phase, practitioners expose athletes to low-intensity (<60% of max speed) linear running and introduce COD activities during the moderate control phase (see figure 3) (4). As the cardio-respiratory focus shifts from aerobic to threshold development during the moderate and high chaos phases, practitioners should adapt the speed and duration of the drills. Athletes should perform general movement and position-specific drills at high intensities and speeds during the moderate chaos and high chaos phases. To optimally prepare recovering tissue to tolerate forces associated with high-speed running and COD, practitioners should include linear, lateral, and multidirectional plyometrics in the rehabilitation program (e.g., repeated lateral depth jumps, and side-to-side high hurdle jumps) (see figure 4).
Figure 4: Multidirectional plyometrics
Biomechanical considerations
Regardless of a muscle group’s ability to generate force, faulty biomechanics could result in injury. Therefore, biomechanical COD, running, or kicking movement analysis may provide insight into load transfer across the groin area and influence training to reduce groin injury risk(9,14). In addition, video analysis to compare biomechanics before the injury, during rehabilitation, and before RTP can provide practitioners with insight regarding the impact of rehabilitation on the athlete's movement quality(9,15).Individualized player management
Most athletes with AGP continue training for long periods before pain forces them to discontinue(2,14). Keeping athletes on the field, court, or track is often an initial goal while managing pain with modified training, manual muscle techniques, and wearing compression shorts(14). However, continued training with symptoms can result in compensatory movement strategies, affecting performance and exposing athletes to additional injury risk(2).There is still considerable variation between individual players’ recovery timelines. In theory, the longer you set the expected timeline, the more likely the athlete will recover fully within expectations. However, the variation in RTP times means that time-based rehabilitation approaches are not optimal. Therefore, clinicians should base the RTP decision on athletes’ function, resolution of pain, and training load tolerance(14).
Conclusion
The Doha classification of groin pain provides practitioners with a helpful guideline on the causes of AGP. Unfortunately, high-quality conclusive research regarding specific treatment modalities is still scarce. However, there is consensus regarding the efficacy of supervised physical training as a treatment modality to optimize athletes’ RTP. Guiding athletes along the RTP and CCC continuums improves their chances of remaining injury-free and performing optimally.References
- Br J Sports Med. 2016;50(19):1181-1186.
- J Orthop Sports Phys Ther. 2018;48(4):239-249.
- Acta Clin Croat. 2014;53(4):471-478.
- Br J Sports Med. 2019;53(18):1132-1136.
- Br J Sports Med. 2015;49(22):1447-1451.
- Br J Sports Med. 2015;49(12):803-809.
- J Sci Med Sport. 2018;21(10):999-1003.
- Sports Med - Open. 2022;8(1):11.
- J Biomech. 2020;99:109474.
- Sports Med. 2017;47(10):2011-2026.
- Phys Ther Sport. 2021;50:22-35.
- Br J Sports Med. 2016;50(14):853-864.
- Supertraining. Verkhoshansky SSTM; 2009.
- Aspetar Sports Med J. 2021;10.
- Co-Kinet J. 2018;(78):7-7.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Further reading
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.






