Optimal Loading in Rehabilitation: finding the ‘sweet spot.’

Skeletal muscle injuries occur when an external force overwhelms the muscle’s ability to generate an equal or greater force. The muscle did not develop the appropriate internal force required to manage the external load for whatever reason. Injury leads to impaired muscle activation due to pain inhibition and reduced muscle activity caused by immobilization(1).
Rehabilitation through exercise is restoring anatomical form and physiological function following an injury(1). Optimal loading is the load applied to structures that amplify physiological adaptation(2). The introduction of varied loads by manipulating different loading variables such as magnitude, intensity, duration, and direction would maximize the neural and cellular adaptation through metabolic, mechanical, and functional mechanisms(2). Practitioners may delay rehabilitation due to the presence of pain; however, exercise is hypoalgesic, although optimal dosage is yet to be established(3).
Loading initiates a cascade of positive biochemical processes(4). Mechanotransduction is how the body converts physiological-mechanical loading into cellular responses(4). Mechanotherapy is simplified into three steps, (1) mechanocoupling – the mechanical trigger, (2) cell-to-cell communication – communication through which the tissues distribute the loading message, and (3) the effector response – cellular level response. The mechanotransduction is weak in the absence of load, and connective tissue is lost(4). When there is a load above the tissue’s set point, there is a stimulus through mechanotransduction, and the body adapts to improve tissue density(4). Tissue loading through skeletal muscle contractions promotes angiogenesis and increased stem cell activity following injury(5). For example, early graded rehabilitation following acute hamstring strain can improve recovery time by three weeks(5).
Figure 1: The envelope of function(7)
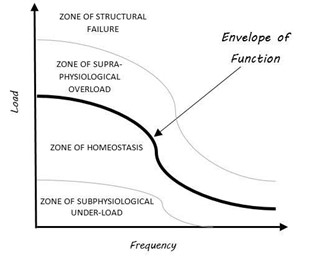
As a system, the human body endeavors to remain in a state of homeostasis. As a subsystem, skeletal muscle is no different. In this context, athletes need to accept, redirect, and dissipate external stimuli to prevent injury(7). When this is unsuccessful, athletes operate at a load beyond their structural capabilities, and failure is likely to cause harm. However, the ability of the muscle to function is not lost entirely. For example, an athlete sustains a grade one hamstring strain and can still run, albeit at a slower speed than their previous maximum effort.
A theoretical tissue homeostasis model exists to conceptualize the pathophysiology of patellofemoral pain. At the heart of this model is the envelope of function; this is the amount of load that a system can safely withstand and transmit without sustaining injury (see figure 1)(7). The injury risk increases when the load or frequency exceeds tissue capacity. This can either be through a gradual supra-physiological overload or a load that causes structural failure. Although this model primarily explains patellofemoral pain, adapting it to acute soft tissue injuries provides an opportunity to develop and progress rehabilitation programs clinically. Through a thorough subjective and objective assessment, practitioners can establish the athlete’s post-injury envelope of function and thus develop an individualized objective outcome measure and practical starting point (see figure 2).
The cellular and neural responses to exercises are essential in promoting healing. This natural, non-pharmacological approach is a positive intervention in rehabilitation(5). However, practitioners are yet to establish the optimal exercise dosage. This is most likely due to the multifactorial nature of injuries, and there is a need for individualized management strategies. The envelope of function allows practitioners to create individualized rehabilitation programs that expose athletes to variable loads and facilitate healing.
Determining an athletes’ current envelope of function starts with a detailed subjective assessment. The athletes’ narrative is the foundation of all rehabilitation programs. Analyzing their aggravating and easing factors should alert practitioners to their current level of function. This helps set a starting point and provides the practitioner with re-assessment tests. Practitioners can use standardized assessment tools to further expand on the degree of injury, but providing the athlete with a test in which they see the direct correlation to their story is essential for further strengthening their buy-in.
Figure 2: Envelope of function in rehabilitation
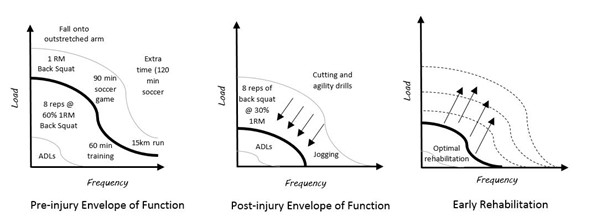
Athletes’ can restore the envelope of function to pre-injury levels through individualized rehabilitation. First, however, practitioners need to prescribe appropriate load to restore tissue capacity.
Ultimately, optimal loading is not a definitive prescription of exercise. Instead, an ever-changing range of movements provides the athlete with the stimulus that promotes recovery and enhances resilience. No two people are the same, and thus no two rehabilitation programs are the same. The complexity of the psycho-social aspects in rehabilitation means that although two athletes may present with the same injury, their response to a load is different. Therefore, practitioners should challenge athletes with an appropriate load. Allow them to develop and progress by providing reassurance and guidance throughout their rehabilitation.
Figure 3: Adapting the envelope of function for soft tissue injuries
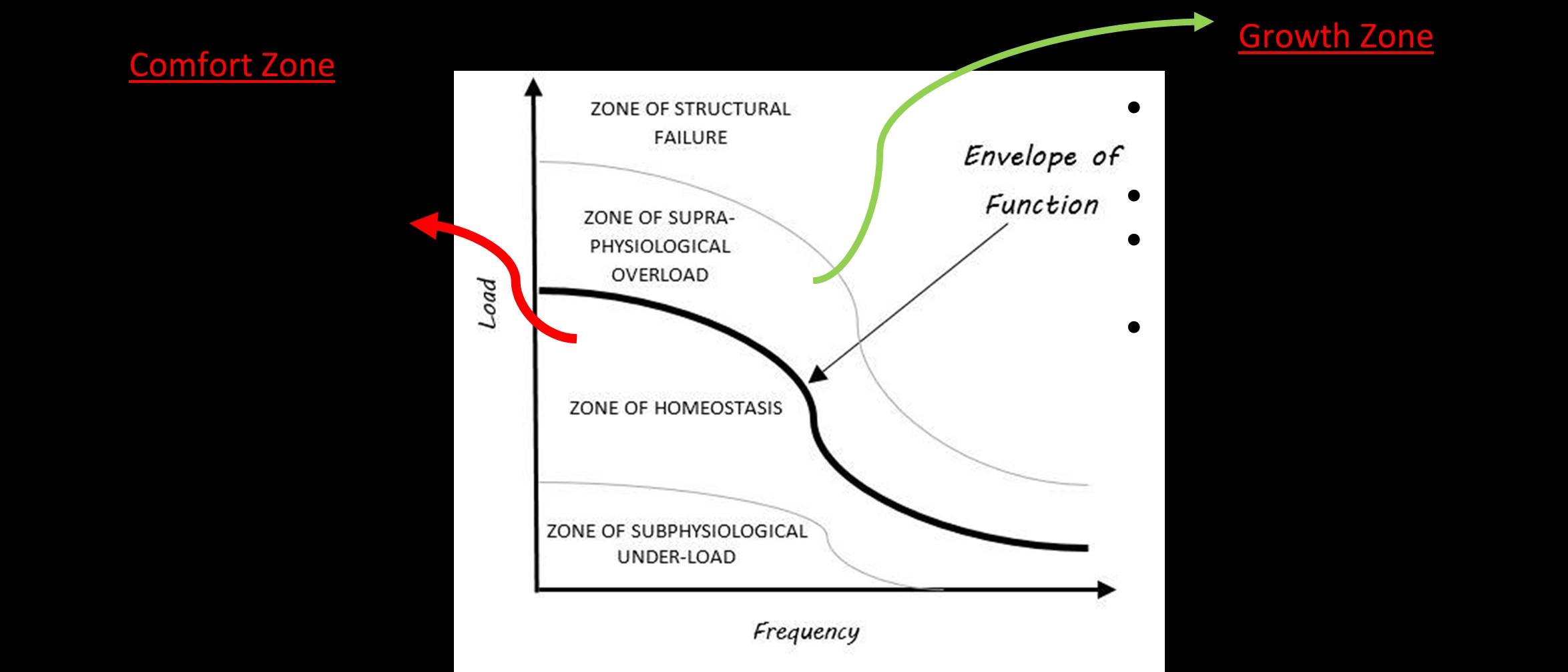
Practitioners can redefine the zone of supraphysiological overload as the “growth zone” and the zone of homeostasis as the “comfort zone.” Using the common analogy that personal development occurs outside one’s comfort zone, athletes may grasp the concept well. If the load is adequate, we grow (physiologically, emotionally, and psychologically). In the “comfort zone,” we stay the same - homeostasis.
Conclusion
The foundation to all successful rehabilitation programs is compliance and consistency. Education is critical so that athletes can take control of their rehabilitation and feel confident enough to amend their programs independently. Successful programs are monitored by a practitioner but controlled by the athlete. Using the envelope of function to find the optimal loading zone provides athletes with the necessary foundational knowledge to take control of their rehabilitation.References
- Frontera, W., 2003. Rehabilitation of Sports Injuries: Scientific Basis. 1st Blackwell Science
- Sports Med. 2015 Mar;49(5):278-9
- J Pain. 2012 Dec;13(12):1139-50
- Br J Sports Med. 2009;43:247–251
- Cell J.2017 Winter; 18(4): 473–484
- The New Eng J of Med. 377(13); 1300-1301
- Clin Orthop Relat Res. 2005 Jul;(436):100-10
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










