Patellofemoral pain: sorted!

Patellofemoral pain (PFP) affects one in six adults with complaints of knee pain(1). What causes PFP remains equivocal. Multiple factors are thought to contribute to anterior knee pain. The elusive origins of PFP may be the reason that 40% of people affected lack significant improvement after a year of treatment(1).
Researchers at the University of Leeds wondered if stratifying patients with PFP might improve outcomes. Stratifying is a concept that is gaining popularity among healthcare practitioners and medical delivery systems. It’s a way to define and sort populations. The approach stems from a need to effectively and efficiently utilize health care resources. If you can identify patients with the highest risk or particular needs, you can quickly deliver the care that they require.
A diagnosis that has many contributing factors, such as PFP, might be best suited for stratification. This method allows practitioners to quickly sort athletes into a group and prescribe a course of treatment that might work best for them. Of course, applying this concept runs the risk of taking a narrow view and perhaps missing a big-picture issue. However the statistics show that the current approach needs improvement. Therefore, this tactic deserves some consideration.
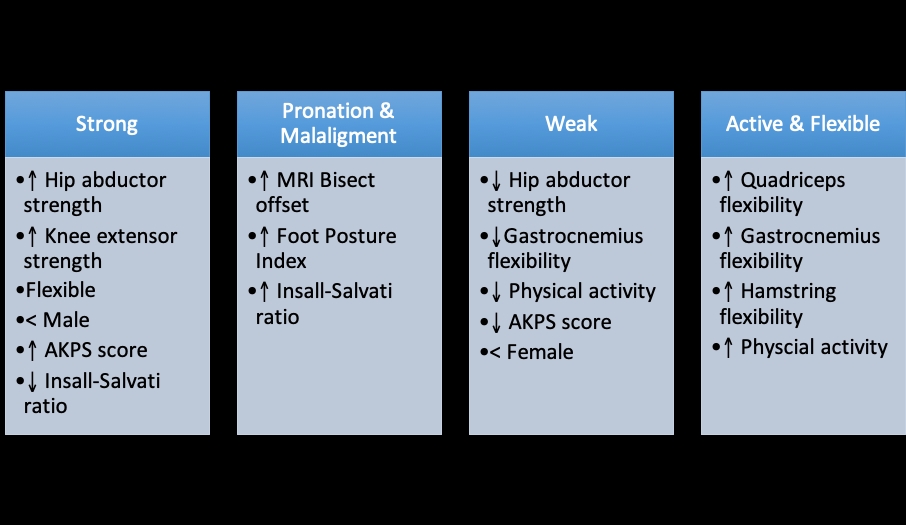
The Leeds team conducted a longitudinal cohort study of 70 adult subjects with diagnosed PFP. They initially evaluated the participants in four key areas: strength, flexibility, joint angle range of motion, and biomechanics and functional characteristics. They then analyzed the baseline data using a two-stage cluster analysis. This statistical approach resulted in 10 groupings based on the results of key data measures. The second stage of clustering found that subjects shared certain characteristics. The researchers sorted the 10 groupings into four sub-groupings according to their common features (see figure 1).
Figure 1: The two-stage cluster approach sorted the PFP subjects into four sub-groupings with shared characteristics.
See article at JOSPT. 2019 July;49(7)538 for an explanation of data collection and scores used.
Due to the small cohort size and other confounding factors, the authors caution against drawing any conclusions from this work. So why bother doing this kind of research, or spend any time even reading the study? Firstly, the findings are similar to that of another research effort by a multicenter study in the UK(2). Those investigators performed six clinical tests of 127 subjects with complaints of PFP. The characteristics they discovered fell into three groupings:
- Strong
- Weak and tighter
- Weak and pronated foot
The two studies combined add evidence to the supposition that PFP is multifactorial. If it were merely due to skeletal misalignment, then all subjects would show bony deviations. If weakness was the primary cause, how does one explain a group with good hip abduction and knee extension strength?
Secondly, it frees clinicians to explore other treatment approaches. For instance, if an athlete complains of PFP but is strong, flexible, and has normal joint range of motion, consider fat pad impingement or an interruption of bone homeostasis. If the athlete is flexible and still maintains a high level of activity, address strength issues, especially in an unlikely muscle like the gastrocnemius. Those with a high foot posture index may be a candidate for an orthotic, while this type of intervention may not help others in the population.
In light of these two studies, a 'one size fits all' treatment approach for PFP seems short sighted. The sorting and application of tailored interventions allow clinicians to begin keeping data of their own. Look for the key characteristics in athletes with PFP and intentionally address those issues in a consistent way. Use standardized functional tests at baseline and discharge and track the effectiveness of the intervention in each subset of patients. Data collected in this way would enable practitioners to choose the most effective mode of treatment and return the athlete to the playing field in record time.
References
- 2019 July;49(7):536-47
- Br J Sports Med.2016 Jul;50(14):873-80
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










