Posterior ankle impingement syndrome

Posterior ankle impingement syndrome (PAIS) is a common ankle injury in athletes who participate in sports that involve repetitive and/or forced plantar flexion(1). It is a painful condition. which limits end of range plantar flexion, and one that can be caused by either soft tissue or bony impingement(2). A clinical diagnosis of PAIS can often be made based on a combination of the patient’s history and physical examination. Treatment for PAIS should initially consist of conservative management; however, if symptoms persist, surgery should be considered. Surgical intervention (either open or endoscopic) has been shown to have very good results, with most athletes returning to their pre-injury levels of sport participation(2).
Anatomy/pathoanatomy
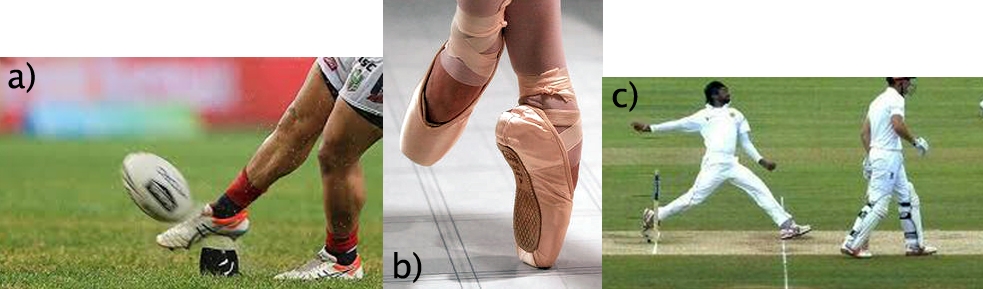
PAIS can be thought of as a group of pathologies that occur due to exposure of the foot to repetitive or forced plantar flexion, and is caused by compression of the structures that lie posterior to the tibiotalar and talar calcaneal articulation(3). PAIS is commonly diagnosed in ballet dancers, but has also been reported in soccer players and cricket fast bowlers(4) (figures 1a-1c shows athletes in these sports placing their ankle in positions of end of range or forced plantar flexion). Multiple soft tissue or osseous structures (either in isolation or in combination) can be compressed within this space.
Figures 1a-1c: Examples of end of range/forced plantar flexion
Osseous causes of PAIS are associated with the lateral (trigonal) process of the talus. Anatomical variations of this structure include a ‘stieda process’ which refers to an elongated tubercle or an ‘os trigonum’. An os trigonum is an anatomical variant that occurs in up 25% of the population, and which may represent a secondary ossification center that has failed to fuse(1). The presence of an os trigonum does not cause PAIS, but it is often present in athletes with PAIS. Injury to the trigonal process can occur with either acute fracture (ie from forced plantar hyperflexion) or chronic injury from repetitive microtrauma, often also resulting in mechanical irritation of the surrounding soft tissues.
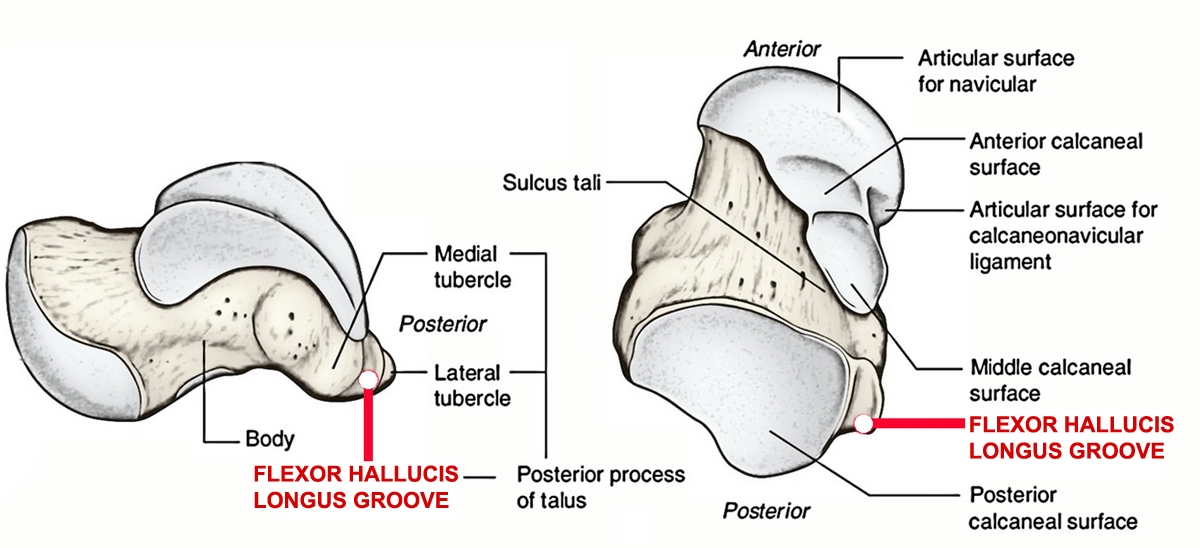
Various soft tissue structures may also cause posterior impingement symptoms. Commonly, the flexor hallicus longus (FHL) tendon may be involved. This is because it sits between the medial and lateral tubercle of the talus (see figure 2), and can become irritated as a result of the underlying abnormal anatomy (ie lateral talar process fracture, stieda process or os trigonum), chronic mechanical trauma or an acute injury resulting in tenosynovitis or tendinosis(3). Other structures that have been implicated in cases of posterior impingement include the capsule, posteroinferior tibiofibular ligament and thickened or inflamed posterior fibers of the deltoid ligament(1).
Figure 2: Location of FHL tendon groove on talus
Clinical presentation
Athletes with posterior impingement present with pain deep to the Achilles tendon and symptoms that typically worsen with activities involving repeated plantar flexion – for example ‘pushing off’ (ie pointe work in ballet dancers), kicking a ball, front foot impact for cricket fast bowlers, wearing high heeled shoes or walking down hill. Athletes may describe a previous trauma or event, but often the symptoms will come on gradually.
When conducting a physical examination, a thorough assessment of ankle ROM and strength should be carried out; activities that require either active or passive plantar flexion will commonly elicit pain. Particular attention should be paid to plantar flexion movement patterns, as a poor movement pattern can predispose to this condition. Ballet dancers with forced turn out (or ‘fishing’) experience increased rotary forces at the ankle; similarly, cricket fast bowlers who overstride at front-foot impact have a higher risk of this condition.
Careful palpation of the posterior ankle can help differentiate PAIS from other pathologies. The site of maximal tenderness is deep to the Achilles tendon - either medial or lateral. Figure 3 shows the common site of maximal tenderness in the athlete with PAIS, comparing it with the site of maximal tenderness of athlete with mid-portion Achilles tendinopathy.
Figure 3: Achilles or PAIS?

The picture on the left shows the common site of Achilles tenderness; picture on the right shows the common site of PAIS tenderness
The definitive test for PAIS is pain on the posterior impingement test. This test requires the athlete to lay prone with the symptomatic knee flexed to 90 degrees. The clinician passively moves the foot into plantar flexion, looking for pain provocation. Overpressure may be required if symptoms are hard to elicit. Clinically, posteromedial tenderness, pain on posterior impingement test that changes with 1stMTP flexion/extension - as well as pain on resisted 1stMTP flexion - indicates involvement of the flexor hallicus longus (FHL) tendon. Conversely, pain in the posterolateral ankle with absence of pain on FHL testing (described above) more likely indicates a pathology involving the trigonal process.
Other differential diagnoses that should be considered when assessing an athlete with posterior ankle pain include:
- Achilles tendinopathy
- Peroneal tendon pathology
- Tarsal tunnel syndrome
- Chronic ankle instability
- Sural nerve pathology
- Lumbar radiculopathy
- Sever's disease
The posterior impingement test will be negative in all these other conditions. Table 1 compares clinical findings of PAIS with some for pathologies that should be considered in athletes with posterior ankle pain.
| Pathology | Clinical tests | Posterior impingement |
|---|---|---|
| Achilles tendinopathy | Tenderness over directly over mid portion or insertion AchillesDiffuse or local thickening of Achilles tendon may be present directlyPain on activities that require ankle dorsiflexion | Site of maximal tenderness deep to Achilles tendonThickening may be present but deep to AchillesPain on activities that require ankle dorsiflexion |
| Peroneal tendinopathy | Peroneal tendon tendernessPain/subluxation on peroneal muscle testing | Site of maximal tenderness medial to peroneal tendonNo pain on peroneal muscle testing |
| Tarsal tunnel syndrome | +ve Tinels test for tibial nerve | -ve Tinels test |
| Sural nerve pathology | Straight leg raise with ankle dorsiflexion/inversion to bias sural nerve | -ve SLR |
| Lumbar spine radiculopathy | Lumbar ROM and neurodynamic testing — SLR or slump | Full Lumbar spine ROM-ve SLR and -ve Slump test |
Imaging is also useful to help differentiate soft tissue or osseous causes. X-ray is generally the initial imaging mode where lateral views may show a stieda process or os trigonum. When the diagnosis is inconclusive or when further information is required, an MRI may be considered(4). MRI findings may include bone oedema, joint effusion, synovitis and/or FHL tenosynovitis and/or chondral injury(4).
Treatment options
The initial approach to treatment of posterior impingement is conservative, with treatment that consists of a period of rest from activities requiring ankle plantar flexion, mobilization of subtalar, talocrural and mid-foot joints, soft tissue treatment of FHL and ankle/calf strengthening as indicated. To help with pain relief, NSAIDs or an ultrasound guided corticosteroid injection around the area of maximal tenderness may also be used with a lateral approach (due to the neurovascular bundle on the medial aspect of the ankle).In cases where the symptoms are manageable, and the athlete chooses to continue playing (ie middle of the season), tape can be useful to restrict end of range plantar flexion. These athletes will still often require a period of rest at a later stage (ie either end of season or when symptoms become too restrictive for them to continue) for symptoms to fully settle. Overall, it has been reported that close to 60-70% of PAIS cases can be resolved with conservative treatment alone(3).
Returning to activities requiring plantar flexion should be guided by findings of clinical examination. Once an athlete has no pain on active or passive plantar flexion, this movement can be gradually recommenced. Athletes whose sports require forced plantar flexion - eg kicking a football and cricket fast bowling - should be symptom free on the posterior impingement test with over pressure before they recommence these activities. The timeframe for this is variable and may be six weeks or even longer.
For athletes who do not respond to conservative treatment and have persistent symptoms, surgery is indicated. The goal of surgery is to excise and/or debride the causative anatomy. This may involve excision of the trigonal process or os trigonum as well as debridement of the surrounding soft tissue structures and hypertrophic tissue(4). Historically this was done through an open procedure; more recently however, endoscopic approaches have become more popular due to a lower complication rate and faster return to sport(4). Operative treatment of dancers and soccer players shows excellent results with close to 80-90% describing good to excellent results(2,3).
Conclusion
Posterior impingement syndrome should be considered in athletes presenting with posterior ankle pain who participate in sports that require repetitive plantar flexion. It is caused by bony or soft tissue impingement (or a combination of both) in the posterior ankle. Conservative treatment is the initial approach and has shown good results. If this fails however, surgical treatment has been shown to have good- excellent results.References
- Yasuli Y , Hannon C, Hurley E and Kennedy J (2016) Posterior ankle impingement syndrome; A systematic four-stage approach. World Journal of Orthopedics. Vol 7 (10) 657-663.
- Rietveld A, Hagemans F (2018) Operative treatment of posterior ankle impingement syndrome and flexor hallicus longus tendinopathy in Dancers: Open versus endoscopic approach. Journal of Dance Medicine. Vol 22 No1 11-18.
- Lavery K, McHale K, Rossy W and Theodore G (2016) Ankle impingement. Journal of Orthopaedic Surgery and Research Vol 11, No 97
- Kudas S, Donmez G, Isik C, Celebi M Cay N and Bozkurt M. (2016) Posterior ankle impingement syndrome in football players: Case series of 26 elite athetes. Acta Orthopaedica et Traumatologica Turcica. Vol 50 649-654.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.








