Sudden cardiac death in athletes: how useful is cardiac screening?

Although the actual incidence of sudden death in athletes is rare (ranging between 1 in 50,000 and 1 in 200,000)(1), the emotional impact on society is high. Many view athletes, especially young ones, as the healthiest segment of the population. Therefore, a sudden cardiac death to an otherwise fit young person is especially traumatic. This contrast fuels the ongoing debate about the best way to screen young athletes to identify those at risk.
Causes of sudden cardiac death
Evidence from the US suggests that the vast majority of sudden deaths in athletes under 35 years of age are due to several congenital or acquired cardiac malformations(2). According to data published by the Minneapolis Heart Institute Foundation Registry (1980 to 2005) and collected from 1435 young competitive athletes, hypertrophic cardiomyopathy is the primary disease of the myocardium (heart muscle) seen in active persons. In this syndrome, a portion of the myocardium is hypertrophied (thickened) without any obvious cause. It is the single most common cause of athlete deaths (responsible for approximately one third of the cases)(2).The next most common causes of sudden cardiac death are a congenital coronary artery anomaly and variant placement of the aortic sinus node. Death resulting from the more common coronary heart disease (CVD) observed in the general population (e.g., arterial blockage due to atherosclerosis, etc.) is comparatively rare. Athletes exercise regularly, which helps protect them from CVD. Also, they tend to be younger and less likely to succumb to the age-related degeneration changes that typify this condition.
Data from the US National Center for Catastrophic Sports Injury Research confirms the multifactorial nature of cardiac pathologies in the young athlete(3). Over two years, 179 cases of sudden cardiac arrest or death were identified (74 arrests with survival, 105 deaths; average age 16.6 years). The most common etiologies include:
- Hypertrophic cardiomyopathy (16.2%)
- Coronary artery anomalies (13.7%)
- Idiopathic left ventricular hypertrophy / possible cardiomyopathy 11.1%)
- Autopsy-negative sudden unexplained death (6.8%)
- Wolff-Parkinson-White (6.8%)
- Long QT syndrome (6.0%)
Significantly, it was estimated that while 56.4% of cases would likely demonstrate abnormalities on an electrocardiogram, a significant proportion would not.
Fit or vulnerable?
Athletes who train vigorously often demonstrate changes in their heart muscle in much the same way they show adaptation in their other muscles; the heart becomes larger, and the walls along the left ventricle become thicker. The volume within the left ventricle increases, and the heart becomes more efficient at pumping blood to the rest of the body.While the actual heart function remains normal in athletes who experience these physiological changes, they may result in what would be considered abnormal electrocardiogram (ECG) readings(4). It’s important for sport physicians to distinguish between normal (and healthy) hypertrophic changes in the heart tissue of an athlete and pathological changes – for example, those brought about by abnormal heart rhythms.
When the heart is structurally sound, it is still possible for sudden cardiac death to occur as a result of an electrical malfunction. This pathology is particularly challenging to detect via screening, and a sudden cardiac arrest may be the first indication that something is wrong. Once diagnosed with an arrhythmia athletes can be managed with medication and an implantable cardioverter defibrillator, a type of pacemaker that automatically detects arrhythmias and shocks the heart back to normal sinus rhythm.
Screening and prevention
The European Society of Cardiology and the International Olympic Committee recommend a pre-participation health screening for athletes. This screening includes a personal and family history, a physical examination, and a 12-lead ECG to examine heart rhythms. In the US, however, the American Heart Association (AHA) recommends only the history and physical portion of the exam, with referral to further testing only for those with significant risk factors. Even in Europe, different countries apply different regulations regarding the minimum complementary tests that should be used in competitive athletes, ranging from ECG to exercise testing or compulsory echocardiography.The explanation for the variation in screening approaches is twofold. Firstly, widespread screening using ECG or echocardiography is time-consuming and expensive. Even if the funds allow, there may not be enough trained medical personnel available to regularly screen the large numbers of athletes who now participate in competitive sport. Then, of course (because no screening technique is foolproof), there’s a debate over just how effective ECG and echocardiography are in identifying at-risk athletes. In particular, there exists the possibility that these techniques can produce false positives (i.e.,indicate a risk where none exists) and even false negatives (i.e., give a clean bill of health where there is a risk).
ECG and echocardiography
The debate over the most appropriate screening techniques to identify athletes at risk of sudden cardiac death is ongoing, particularly as there is currently no universally accepted screening protocol. In 2008, US researchers investigated the use of EGC and echocardiography screening to detect hypertrophic cardiomyopathy in highly trained athletes(5). The authors concluded that overall, the prevalence of hypertrophic cardiomyopathy in highly trained athletes was infrequent.The structural and functional changes associated with hypertrophic cardiomyopathy tend to weed out most individuals from competitive sports. The study also concluded that screening athletes with echocardiography was not cost-effective but that electrocardiography was useful in selecting out those who may have pathological left ventricular hypertrophy for subsequent echocardiography.
A 2012 review study examined pre-participation screening for the detection of intrinsic structural or electrical cardiovascular disorders that predispose an athlete to sudden cardiac death(6). It concluded that there was considerable evidence suggesting that screening athletes with only a history and physical examination leave most athletes with a serious underlying cardiovascular disease undetected. This approach cannot, therefore, adequately achieve the primary objective of screening. The authors added:
“Pre-participating cardiovascular screening inclusive of an ECG greatly enhances the ability to identify athletes at risk and is the only model shown to be cost-effective, and may reduce the rate of sudden cardiac death.”
A focused approach
The above findings appear to suggest that ECG screening is not only the preferred method but also in itself sufficient for detecting cardiac pathologies in athletes. However, other data indicate that a technique known as focused echocardiography canbe a valuable tool, especially when combined with ECG data(7). Focused echocardiography uses a miniaturized, portable echocardiography machine. The trained operator (who doesn’t need to be a cardiac physician) rapidly assess key aspects of cardiac function, including pericardial effusion, chamber size, global cardiac function, left ventricle size, and ventricular function providing considerable potential for rapid and effective screening in the field.In a 2014 study, 65 male collegiate athletes (aged 18 to 25 years) were screened with a history and physical examination, ECG, and focused echocardiography performed by a non-cardiologist sports medicine physician. In particular, the (physician-operated) focused echocardiography was performed to look for hypertrophic cardiomyopathy and aortic root dilatation. Athletes screening positive were referred to a cardiologist.
The screening found suspect results in six athletes. After referral to a cardiologist, these athletes were cleared for sports participation. Importantly, no athlete screened positive by focused echocardiography alone. The conclusion was that focused echocardiography reduced the referral rate for hypertrophic cardiomyopathy by 33% and obtained measurements statistically similar to those of formal echocardiography.
More evidence
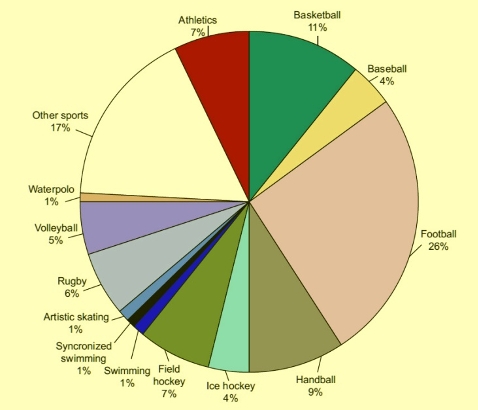
Another study of 2688 athletes from different sporting disciplines (see figure 1) provides persuasive evidence for adding echocardiographic imaging to a screening program(8). In this study, all athletes underwent a cardiovascular evaluation consisting of the following:- Family and personal history
- Physical examination
- ECG
- Echocardiogram
- Maximum exercise testing
Most echocardiography examinations (92.5%) were normal and showed no cardiac disease. However, changes were seen on the echocardiogram of 203 participants (7.5%). The variation most frequently found was left ventricular hypertrophy with 50 athletes (1.86%) having left ventricular hypertrophy, using an interventricular septum cut-off measure of 12 mm. The incidence was reduced to 30 (1.11%) if the cut-off was increased to 13 mm. Thus, 20 participants showed left ventricular hypertrophy that could be considered physiological. However, none of the ECGs of these athletes met the diagnostic criteria of hypertrophic heart muscle disease.
Physicians recommended that four athletes stop sports completely. Two of these four athletes had hypertrophic heart muscle disease. The third individual had a pectus excavatum that compressed the right ventricle. The fourth subject showed significant pulmonary valve stenosis.
The critical point of this study is that the medical history, physical examination, or 12-lead ECG didn’t detect any of these problems. The additional echocardiography provided a more comprehensive evaluation of the cardiac risk than the ECG screening alone. It also diagnosed four athletes with a risk of sudden death and three athletes with a disease that required a specific treatment or follow-up.
Figure 1: Sports practiced as a percentage of the total number of athletes evaluated(8)
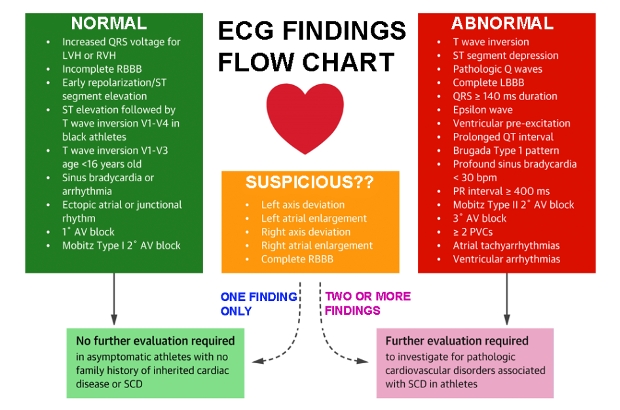
Maximizing ECG specificity
While ECG screening can detect vulnerable athletes, it often produces false-positive results which, when referred to a cardiac specialist, are subsequently cleared(6,9). While a ‘better safe than sorry’ approach seems reasonable, false positives are time and resource consuming and create unnecessary worry in the athlete’s mind. A new set of ECG interpretation criteria hopes to provide ECG interpretations that distinguish common physiological adaptations in athletes from distinctly abnormal findings (suggestive of underlying pathology)(9).The International Recommendations (see figure 2), provide updated ECG interpretation standards based on new and emerging research. These guidelines direct the appropriate evaluation of ECG abnormalities for conditions associated with SCD in athletes. The recommendations aim to reduce the number of false-positive results without reducing the sensitivity of the screening process. In a study at the University of Washington, two experts in the field of sports cardiology re-examined ECGs from 5258 NCAA athletes who underwent pre-sport screening by using both the Seattle (previous) and the International (new) ECG interpretation criteria(10). Each ECG was classified as normal or abnormal, and the specific ECG abnormalities noted. The total number of ECGs flagged as abnormal by expert over-read decreased from 158 (3.0%) using the Seattle criteria to 83 (1.6%) using the International criteria.
Figure 2: The (new) International ECG screening criteria(9)
In summary
Pre-participation screening is required to reduce the risk of sudden cardiac death among athletes. A family and personal history plus a physical examination screening are considered insufficient to detect some forms of serious underlying cardiac disease. Athletes engaged in competitive sport should also undergo regular ECG screening, ideally using the International Recommendations for interpretation. Evidence also suggests that the addition of focused echocardiography to a screening program (directed at excluding specific diseases that cause problems for athletes) seems appropriate, especially as this type of echocardiography does not need to be performed in a hospital setting by an experienced radiographer.References
- Heart. 2009;95:1409-1414
- Circulation. 2007; 115: 1643-1655
- Clin J Sport Med. 2020 Jul;30(4):305-314
- Circulation. 2010;121:1066-1068
- J Am Coll Cardiol. 2008 Mar 11;51(10):1033-9
- Prog Cardiovasc Dis. 2012 Mar-Apr;54(5):445-50
- J Ultrasound Med. 2014 Feb;33(2):307-13
- Rev Esp Cardiol. 2014 Apr 8. pii: S0300-8932(14)00101-8
- J Am Coll Cardiol. 2017 Feb 28;69(8):1057-1075
- J Electrocardiol. Sep-Oct 2019;56:81-84
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.






