Uncommon injuries: Posterior interosseous nerve dysfunction - a cause of lateral forearm pain

Lateral elbow pain around the extensor compartment of the forearm is typically attributed to lateral epicondylitis. Known also by its common name of tennis elbow, this condition affects the common extensor tendons that originate on the lateral epicondyle of the humerus(1). Injuries to the proximal radioulnar joint may also produce pain and dysfunction in this area. Though less common, compression neuropathies of the radial nerve, specifically the deep branch of this nerve known as the posterior interosseous nerve (PIN), create a deep ache in the lateral forearm and lead to weakness in wrist and finger extension. Compression of the PIN occurs in athletes who repeatedly exert grip strength with excessive pronation and supination movements. The terms radial tunnel syndrome or resistant tennis elbow, coined in the 1970s, reflect the link between compression of the PIN and pain in the upper forearm(2).
Relevant Anatomy
The PIN is a branch of the radial nerve. The radial nerve originates from the nerve roots of C5-T1 and exits the posterior cord of the brachial plexus. As the radial nerve courses down the upper arm, it divides in the proximal forearm into the superficial sensory branch and the deep motor branch that passes through the Arcade of Frohse to then course between the heads of the supinator muscle to form the PIN(³) (see figure 1). The extensor carpi radialis longus and the brachioradialis receive motor innervation from the radial nerve just before it passes through the Arcade of Frohse, and thus are not directly supplied by the PIN.Figure 1: Anatomy of the Posterior Interosseous Nerve
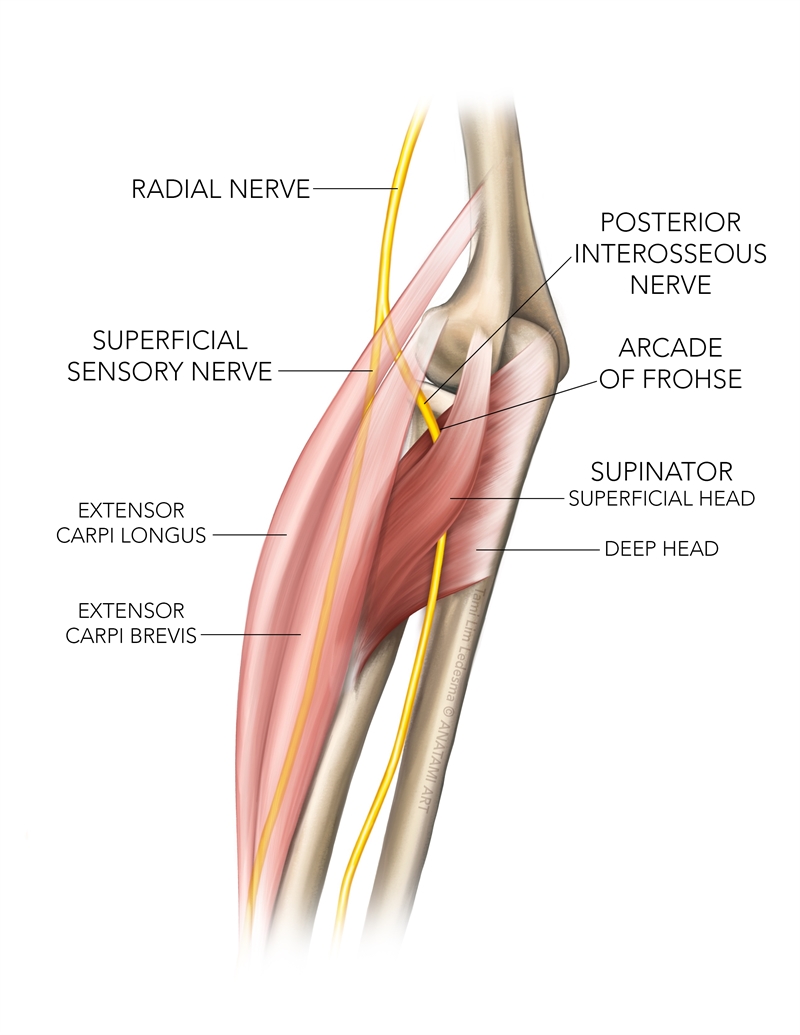
Another important anatomical landmark, the radial tunnel, extends from the head of the radius to the inferior border of the supinator. The walls of the tunnel are formed by the supinator, extensor carpi radialis longus, extensor carpi radialis brevis and brachioradialis muscles(⁴). The radial tunnel is proximal to the supinator muscle, and compression of the radial nerve in this area can lead to other pathologies that mimic PIN compression.
The PIN is a motor nerve that supplies these muscles of the forearm(3):
- Supinator
- Extensor carpi ulnaris
- Extensor carpi radialis brevis (ECRB)
- Extensor digitorum communis
- Extensor digiti minimi
- Extensor pollicis longus
- Extensor pollicis brevis
- Abductor pollicis longus
- Extensor indicis
Because the PIN is primarily a motor nerve, compression often leads to weakness with no pain. However, the PIN also innervates the periosteum of the radius, the interosseous membrane, and the dorsal wrist capsule(3). This likely explains the deep ache in the forearm felt by the sufferer of PIN entrapment.
Injuries to the PIN
Posterior interosseous nerve syndrome is a compression neuropathy of the PIN, which innervates the extensor compartment of the forearm. This syndrome results from trauma (such as incurred by a fracture of the radial head), or spontaneous compression. Known sites of compression by the supinator muscle include the Arcade of Frohse and the radial tunnel(5). Compression at these locations is sometimes called supinator syndrome and does not cause sensory changes(6). Traction on the nerve by repetitive pronation and supination movements and compression by a host of space-occupying lesions can also cause PIN syndrome(5,7-9). Females suffer from PIN syndrome more than males, and the right side is more commonly affected than the left(9). Swimmers, tennis players, and powerlifters are vulnerable to PIN syndrome(5,10).Many other causes of compression neuropathy of the radial nerve besides PIN syndrome exist. Location, causes, and signs of other compression syndromes that should be considered in a diagnostic evaluation include(11-15):
1.Lateral elbow joint at radial head
a)Caused by OA, fibrous bands or synovitis of the radiocapitellar joint.
b)Compression here may cause sensory changes.
2. Leash of Henry
a) An arcade of blood vessel branches of the recurrent radial artery at the neck of the radius.
b) Compression here may cause sensory changes.
3. Fibrous edge of ECRB
a) The medial proximal edge of the ECRB.
b) Compression here may cause sensory changes.
4. Wartenberg’s Syndrome
a) Compression of the superficial sensory radial nerve between the brachioradialis and the extensor carpi radialis longus during forearm pronation.
b) Compression here causes sensory changes and pain over the dorso-radial hand.
5. Compression of the selective motor fascicles of the radial nerve
a) Occur in the upper arm above the elbow.
b) Mimic PIN compression symptoms.
6. Radial Tunnel Syndrome
a) The maximal site of tenderness is usually 3-5 cm distal to the lateral epicondyle, further down than typical tennis elbow symptoms.
b) The distinct feature is forearm pain with no motor weakness. May have pain on resisted supination.
Signs and Symptoms
Athletes suffering from PIN compression neuropathy often initially complain of weakness in grip strength during sports. This weakness may progress to the fingers, thumb, and wrist, with a deep ache in the extensor compartment of the forearm. It may imitate the more common tennis elbow pathology at this point as often the signs and symptoms of both overlap. However, the key features are(5):- Insidious onset of weakness in finger extension at the MCP joint.
- Weakness in extension and abduction of the thumb.
- No sensory loss but a deep ache in the proximal forearm may develop.
- Often associated with lateral elbow pain that is exacerbated by pronation and supination.
- Wrist drop is not a feature as the extensor carpi radialis brevis and longus remains intact.
- When asked to make a fist, the wrist may deviate radially due to extensor carpi ulnaris weakness(7).
- Positive Tinel’s sign in severe injuries(16).
- Possible positive radial nerve tensioning test.
Diagnostics
Medical investigations to consider:- Electromyography (EMG).
- Nerve conduction studies (NCS) to detect denervation of the muscles innervated by the PIN(17).
- Magnetic Resonance Imaging (MRI). Reveals evidence of muscle denervation (seen as muscle edema and loss of muscle volume with fatty changes) in the muscles innervated by the PIN(18).
- Magnetic Resonance Neurography (MRN) allows detection of nerve lesions seen as increased T2-weighted signals, which help localize the lesion(11).
Treatment
Identifiable PIN compression neuropathy with definitive features of finger, wrist, and thumb extension weakness and confirmed through investigative radiology typically responds to conservative treatment. Practitioners recommend a trial of rehabilitation for three to six months to stimulate the recovery of wrist and finger function.The recommended conservative management includes:
1. Splinting
Use a wrist/finger splint (nighttime +/- day time) to protect finger/wrist extension.
2. NSAIDS/corticosteroid injection
Recommended for suspected nerve irritation and if the athlete complains of a deep ache along the deep periosteum of the radius.
3. Activity modification
Initially, the athlete will be instructed to avoid activities that involve strong grip positions to allow time for the nerve to recover.
4. Active finger extension, wrist extension (with an ulnar deviation bias) and thumb extension/abduction exercises
Augmented with electrical muscle stimulation if needed.
5. Radial nerve mobilizations
In the event the athlete does not respond to conservative treatment, then decompression surgery is the final option. The PIN decompression occurs in and around the known impingement zones such as(7):
- Fibrous bands superficial to the radiocapitellar joint
- Fibrous edge of the ECRB
- Leash of Henry (radial recurrent artery)
- Arcade of Frohse
- Distal edge of the supinator.
Conclusion
The radial nerve is susceptible to compression and injury around the elbow joint and forearm. Compression neuropathy of the deep branch called the PIN is an uncommon cause of deep forearm ache in the athlete with associated finger extension weakness and thumb extension/abduction weakness. The most common site of compression of the nerve is at the Arcade of Frohse. It may occur in athletes who overuse pronation and supination movements while using a substantial grip. Conservative management usually shows improvement in wrist and finger extensor function within three to six months. Part II of this series will delve into the treatment of nerve-based pathologies and offer strategies for improving PIN syndrome. If conservative treatment fails, then consider decompression surgery.References
- The American Journal of Medicine, 2013. 126(4), 357.e1-357.e6
- J Bone Joint Surg Br. 54(3):499-508
- J Hand Ther. 2006; 19(2):180-4
- J Bone and Joint Surgery (Br). 1968. 50; 809-812
- Tohoku J. Exp. Med. 2001. 193(3):251-4
- Hand Clin. 1992;8(2):345-57
- 1990;27(3):397-402
- Neurosurg. 2006;104(5):766-77
- Arthritis Rheum. 2011;40(6):576-9
- Clin Plast Surg 2003;30: 155–173, vi
- Int Orthop. 1998;22(2):102-6
- Journal of the Peripheral Nervous System. 2002. 7:229–232
- 2016. 87(18):1884-1891
- Arch Bone Jt Surg. 2015;3(3):156-162
- J Am Acad Orthop Surg. 1998 Nov-Dec;6(6):378-86
- J Hand Surg Am. 2009. 34(10):1906-14
- Indian J Radiol Imaging. 2014;24(3):217-24
- Am Fam Physician. 1983; 28(5):133-43
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Further reading
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.