What causes patellofemoral pain?

As Karen Litzy explains in her recent article, pain is a complex phenomenon. For a time, it was considered the fourth vital sign. However, it’s an unreliable symptom. Unlike blood pressure or pulse, pain is subjective. It’s expression and perception differs among genders, cultures, socioeconomic status, race, current emotions, and just about every other aspect that makes one individual different from another. Everyone who experiences an ACL tear, for instance, will not experience the same level of pain, nor will they express it in the same way.
For this reason, pain should be noted and acknowledged, but not trusted as an indication of the extent of injury. In other words, there isn’t a direct correlation between the perception of pain and tissue damage. Physicians from West Virginia and California acknowledged this fact in a review paper on patellofemoral pain (PFP)(1). This common complaint lacks a specific cause, however, athletes often complain of it hurting more with long periods of knee flexion (as in the position of catchers and cricketers) or when going up and down stairs.
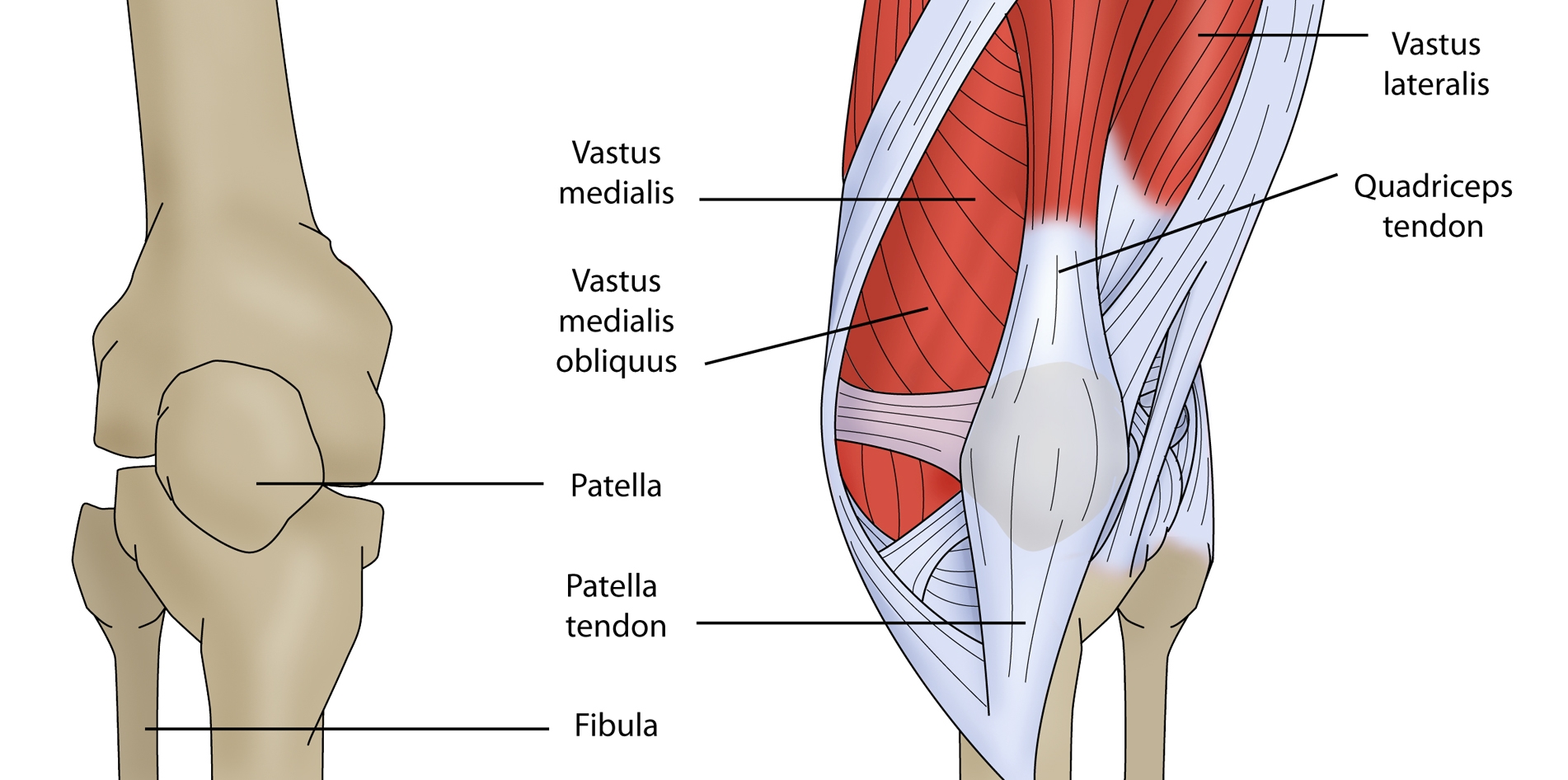
These researchers contend that PFP isn’t part of a syndrome, as sometimes portrayed. There isn’t an agreed upon etiology for the pain experienced in the anterior knee (see figure 1). Therefore, some prefer the term anterior knee pain (AKP) as the patellofemoral structures may not even be the sources of the pain. These authors contend that AKP is caused by an interruption in the homeostasis of the musculoskeletal structures around or within the knee joint.
Figure 1: Anterior knee anatomy
The authors define homeostasis as,
“maintaining relatively stable and asymptomatic physiologic conditions in all organ systems under fluctuating environmental conditions.”(1)
The researchers coined the term “envelope of function” to signify that magnitude of load or frequency of load where the tissues are able to restore homeostasis without incident. When the load is excessive and thus outside the “envelope of function,” as with a sudden increase in training frequency, or when an injury occurs, the tissues can no longer maintain their homeostatic state. They hypothesize that it is the loss of homeostasis within the tissues that causes the individual to experience PFP. Thus, once homeostasis is restored, PFP should improve. With this explanation of the origin of PFP, it makes sense to avoid treatment options that make the pain worse.
Traditional causes of PFP and the new paradigm
The term chondromalacia patella describes a softening of the patella’s articular surface. This phenomenon is often cited as the cause of PFP. The authors of this review take a ‘common sense’ view of this etiology, stating that no amount of conservative care can change the bony structure. Therefore, how is it that athletes improve with a therapy-based intervention?Furthermore, the articular cartilage lacks sensory innervation. Therefore, it can not be a source of pain in and of itself. It can, however, redistribute the load bearing, transferring more stress to the subchondral bone which is significantly innervated with sensory fibers. However, studies show that significant loss of joint integrity and alteration of load bearing doesn’t always correlate with pain, as in those with asymptomatic osteoarthritis.(1) This then calls into question the presumption that findings of chondromalacia patella are the cause of the PFP.
The other oft implicated cause of PFP is patellar misalignment or faulty tracking. Again, studies show that misalignment frequently exists without any symptoms at all.(1) Furthermore, many of those with misalignment who experience PFP respond positively to conservative care, which does nothing to change structure.
In regards to patellar tracking, the authors acknowledge the success of McConnell taping to relieve anterior knee pain. However, they doubt it has to do with actual change in the structural anatomy which improves the movement of the patella. Rather, they hypothesize that it relieves the pressure on sensitive tissues that cause the pain.
What’s likely causing anterior knee pain
The authors of this review speculate that the impingement of highly innervated structures, such as the fat pad and the synovium, is the likely source of pain emanating from the anterior knee. Like when one bites the inside of their cheek and the site of trauma swells, leading to repeated biting and more trauma, irritated or impinged synovium hypertrophies. The more it expands, the more likely it is to suffer repeated impingement and trauma. The byproducts of the breakdown of articular cartilage from excessive load can also lead to synovial inflammation. McConnell taping, they surmise, simply pulls away the tissue offering relief similar to pulling the cheek out of the way of the offending teeth.Another theory is that the interosseous homeostasis of the patella itself is interrupted. Studies using bone scans and positron emission tomography (PET) scans detect osseous changes within the patella in symptomatic individuals.(1) The bony structure returns to normal as the symptoms resolve. The patella is highly innervated, therefore, when the load exceeds the capacity of the bone, the damage and resulting interruption of homeostasis, likened to the stress reaction seen in other bones susceptible to stress fractures, may be the source of pain.(1)
Other innervated structures surrounding the anterior knee may also cause pain. Less likely but still possible sources of pain are:
- patellar and quadriceps tendons;
- joint retinaculum;
- patellar bursa;
- intramuscular trauma to the quadriceps;
- quadriceps inhibition or weakness leading to alteration in loading;
- neuroma/neuropathy of the infrapatellar branch of the saphenous nerve;
- decreased flexibility in the hip and knee musculature altering force distribution;
- intra-articular swelling;
- weakness in hips or core altering force distribution and overloading the patellofemoral structures.
Treatment
In treating PFP, the authors cite the axiom, “First, do no harm.” Following this principle, and assuming that pain is caused by an interruption of homeostasis, it makes sense to avoid treatments that make the pain worse. All treatments should aim to return the involved tissues to their homeostatic state. Therefore, the authors recommend modifying activity to stay within the pain-free “envelope of function” until changes in strength and flexibility enable the system to withstand more loading.While discomfort and muscle soreness are to be expected with exercise and stretching, avoid eliciting more AKP from the athlete. Doing so may require significant patient education and an understanding of what activities make the pain worse. Cryotherapy can be used twice per day to help manage pain. Use of non-steroidal anti-inflammatory medications as directed helps modulate pain and inflammation. Surgical intervention may be considered for those who do not respond to conservative management, however, healing and a return to homeostasis can take months to years to achieve.(1)
Reference
- Am J Orthop (Belle Mead NJ).2017 Mar/Apr;46(2):92-100.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










