A clinicians guide to side strains in cricket fast bowlers

Side strains have been reported in a variety of sports, including javelin throwers, baseball pitchers, tennis players, golfers, and cricketers. This article, however, focuses on side strains in cricketers. Australian cricket data (based on both state and national players) reports that in the 18 cricket seasons up to 2013-2014, side strains had the second highest incidence and the third highest prevalence of all injuries that resulted in players missing games(1). Over 90% of the reported side strains (described as acute onset lateral trunk pain and occur during the bowling delivery) in cricketers over the last 20 years have occurred in fast bowlers(1).
What is a side strain?
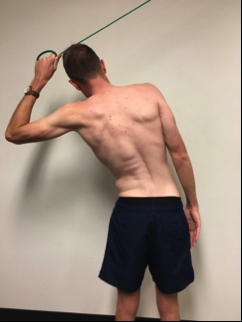
A side strain in cricket occurs most commonly when bowling. Fast bowlers will describe that during a single delivery, they felt sudden onset, sharp lateral trunk pain on the side contralateral to their bowling arm(2). On most occasions, the bowler is unable to continue bowling (although this is not always the case) and often the player will leave the field. The mechanism of injury is thought to be related to the bowler; their quest to increase ball velocity, vigorously pulling the front arm (contralateral side to their bowling arm) down causing a strain (see figure 1).Age and intensity are also potential risk factors for a side strain(1). Younger bowlers (under 24years of age) have been shown to be twice as likely to suffer injury as those aged between 25-29 and 3 times more likely than bowlers over 30 years(1). Side strains also occur more commonly in the early part of the season and most occur during early season matches. This suggests that changes in intensity from training to competitive games may contribute to the likelihood of injury in the early parts of a season. With most recurrences of side strain occurring within a season, increases in intensity may also be a risk factor in recurrences(1). Interestingly, there seems to be no additional increase in risk if a side strain is reported in a previous season.
Figure 1: Strain mechanism

Clinical presentation
The fast bowler will commonly report an acute localized sharp lateral trunk pain (often in the mid-axillary line) that occurred during their delivery. They may also describe pain with breathing, coughing and sneezing, and they can be very uncomfortable moving around especially rolling over in bed. The pain may radiate slightly into the abdominal area. From this description alone a side strain is highly likely.Clinical tests
1) Palpation
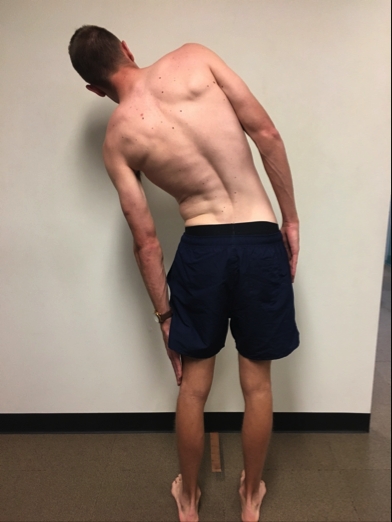
A player with a side strain will be extremely tender over one or more of the lower four ribs (most commonly in the mid-axillary line).2) Lateral flexion range of motion (ROM) test ROM
The player stands side on to a wall with feet pelvis width apart, and the pelvis and the lateral border of one foot up against a wall. The hand closest to the wall is placed on their head. With the pelvis remaining in contact with the wall, the player is then asked to purely laterally flex away (avoiding truck flexion or extension) from the wall as far as they can and the therapist measures how far from the floor their middle finger can reach down their leg. This test in the early phase is often both restricted and painful. The therapist measures both the distance and where the restriction is felt – for example, ‘jamming’ on the ipsilateral side or ‘stretch’ on the contralateral side. These results can then be compared with the non-injured side and/or previous measures. This test is also useful as a monitoring tool throughout a season to determine ‘normal range and feeling’ and may pick early signs of tightness. Post-injury, players should be able to return to full lateral flexion range of motion and their normal restriction feeling.Lateral flexion ROM test

3) Side pain contraction tests
(Note - these tests are progressive with stage 1 being the easiest and stage 3 the hardest. Once a player is pain-free on one stage, progress the testing to the next stage.)Stage-1 side pain contraction test

Stage 1: Isometric shoulder adducted in 90-degree abduction- Player places hand of side that is injured on head, with elbow remaining in line with body in coronal plane. The therapist places hands just proximal to elbow and the player attempts to adduct shoulder. The therapist pushes up as the player pushes down to ensure an isometric test.
Stage-2 test

Stage 2: Isometric shoulder adduction from elevation- Player fully elevates the hand of side that is injured. The therapist places hands just proximal to elbow or wrist, and the player attempts to adduct shoulder. The therapist pushes up as the player pushes down to ensure an isometric test.
Stage-3 test

Stage 3: Isometric shoulder adduction and ipsilateral side flexion from full shoulder elevation and contralateral side flexion- Player fully elevates hand of the side that is injured and then laterally flexes truck to the contralateral side. The therapist places hands just proximal to wrist (or elbow) and the player attempts to adduct shoulder and lateral flex trunk towards the injured side. The therapist pushes up as the player pushes down to ensure an isometric test.
4) Alternative contraction tests
Sit up/crunch test

Sit up/crunch with resistance- Player lies in a crook lie with hands across chest. They then do a straight crunch. To further load the oblique muscles, a rotation can be added to the crunch. If these are not painful then the therapist may add resistance to increase the demand of the test.
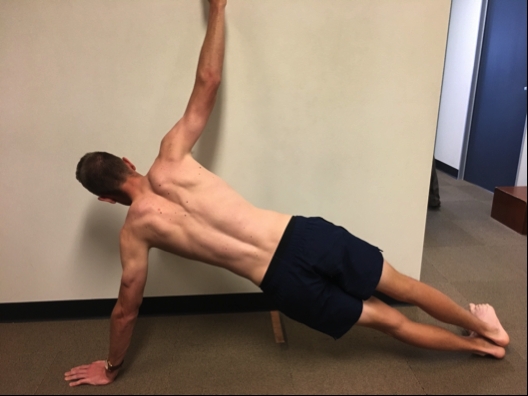
Side plank on a bench

Side plank- This test can be very painful initially. The side plank is not only a good assessment test, but it can also be used to monitor and progress treatment. Initially, a side plank may only be able be possible on knees or with elbows on a bench (height of bench and time should be recorded). As a player progresses the difficulty of the test can be increased by increasing time of hold or decreasing the height of the bench until they are on the floor. Alternatively, increase the difficulty by asking the player to do it on their hands rather than their elbow.
Side plank on hands
5) End-stage pain provocation test: Ipsilateral side flexion combined with a deep breath (inspiration) and progressed to ipsilateral side flexion with a cough
Once a player has no pain on breathing, coughing, or full range of motion, combine these movements. Player fully lateral flexes to side of pain and takes as deep a breath as possible. Note any pain. If this is pain-free then add a cough in full side flexion. If this test is pain-free, progress the player to some bowling at moderate intensity.End-stage provocation test
Imaging
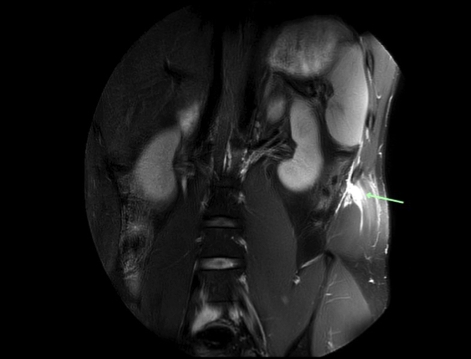
Diagnosis of a side strain is generally a clinical diagnosis based on the description of injury and positive findings from the clinical tests outlined previously. Imaging is however useful in determining the extent of damage and exact structures involved(2). Ultrasound can be used but MRI is the modality of choice. On MRI, an acute side strain is characterized by a high signal on the T2 image at the muscle, rib/costal cartilage interface, and often shows a complete or partial tear of the abdominal musculature(2). The internal oblique at its attachment onto the 11thrib is the most common muscle injured. However, pathology has also been reported in external oblique, transversus abdominus, and abdominal muscle attachments of the 9-12thribs(1,2). MRI imaging may also show rib or costal cartilage damage, including bone stress, bone avulsion or periosteal stripping(1). With these injuries, hematoma may be seen tracking between the internal and external oblique musculature(1). Figure 2 shows an MRI image of an elite level fast bowler with a tear of the internal oblique muscle as it attaches onto the 11thrib.Figure 2: MRI imaging of internal oblique tear
Differential diagnosis
Consider the following diagnoses when assessing a bowler with side pain:- Costoiliac impingement - This occurs as a result of a decrease in space between the lower ribs and pelvis, and may be due to either a hypertrophied internal/external oblique muscle, rib hypertrophy or a hypersensitive scar from a previous side strain.
- Referred pain - from thoracic spine and/or either costotransverse or costovertebral joints.
| Side strain | Costoiliac impingement | Thoracic spine referral | |
|---|---|---|---|
| Palpation | Very tender mid axillary line and along rib | Tender along rib in mid axillary line | Minimal tenderness |
| ROM test | Pain and restriction both lateral flexion toward and away | Most painful with lateral flexion toward | Can be painful on either lateral flexion toward and/or away |
| Contraction tests-Stage 1-3 | Painful and weak | Slightly painful, often good strength | Not significantly painful or weak |
| LF toward and cough | Very painful | Very painful | May be painful |
Treatment
In the early stages, the main aim is to decrease pain especially if breathing, coughing, and sneezing are painful. This can be done through the use of pain-relieving medication in the acute phase. When the player can deep breathe and cough then cardiovascular training can commence - initially with biking or walking and then progressing to running as pain allows.Once tenderness starts to resolve, manual therapy can also be useful, including:
- Soft tissue work throughout abdominal musculature especially obliques, and rectus abdominus.
- Thoracic spine and rib mobilisation.
- Gentle stretching to the contralateral side, combined with deep-breathing drills to help expand ribs.
- Dry needling.
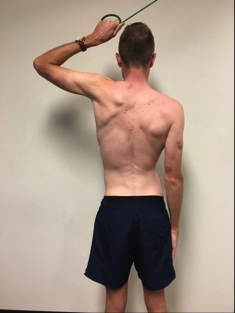
Start strengthing exercises as soon as pain allows. This should commence with isometric exercises, and progress to slow through-the-range exercises. Finally, higher-speed drills and sport-specific drills will help prepare for the intensity of bowling. Some examples of useful exercises for each of these stages are:
- Isometric: side planks – start on a bench and progress to floor (as per the assessment test)
- Slow isotonic: move through side range with band or pulley machine (see figure 3).
Figure 3: Slow isotonic conditioning exercise using band
Return to sport criteria
A player can commence a return to bowling plan when they have:- no pain on breathing, coughing or sneezing
- full ROM and no pain with ipsilateral lateral flexion
- no pain and good strength with stage 1-3 contraction tests
The length of time to return to play from this injury varies considerably with reports ranging from one to seventy days(1). Rehabilitation should be guided by a player’s symptoms rather than based on scan results or a specified time. Within-season recurrence rates are high for this injury, and as such, the return to bowling plan requires a graded return to both volume and intensity.
| BOWLING PROGRAM Balls, Run | INTENSITY | BALL SPEED | WEEKLY BALLS |
|---|---|---|---|
| 24, 1/430, 1/4 | 60% | 105-110 KPH | 54 |
| 18, 1/412, 1/2 | 70% | 110-115 KPH | 90 |
| 30, 1/2 | 70% | 110-115 KPH | 90 |
| 18, 1/212, 3/4 | 70% | 1150120 KPH | 90 |
| 30, 3/4 | 80% | 120-125 KPH | 90 |
| 18, 3/4 12, full 80% | 80% | 120-125 KPH | 90 |
| 30 full 80% | 80% | 125-130 KPH | 90 |
| 18, 80%12, 100%2430 | 90-100% | 125-130 KPH | 114 |
| 30 | 90-100% | 130-135 KPH | 114 |
| 483072 | 100% | 135 KPH | 150 |
Conclusion
Side strains are a common and significant injury to cricket fast bowlers as they often require considerable periods of rehabilitation and inability to play. The clinician should be aware that this injury has a high ‘within-season’ recurrence rate and a graded return to high-intensity bowling is an integral part of the rehabilitation process. Further studies are required to determine risk factors and the relationship between imaging findings and time frames for return to play.References
- J Sci Med Sport. 2017 Mar;20(3):261-266
- British Sports Med 2004 38 (5): e21
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.








