Autoregulation: The solution to the rehab programming puzzle

Training prescription is a delicate balancing act of tissue-loading. Overload a client, and they may suffer setbacks in the form of pain, swelling, and tissue damage. But, conversely, underloading will affect the development of the physical capacities necessary for performance in their sport.
Exercise prescription conundrum
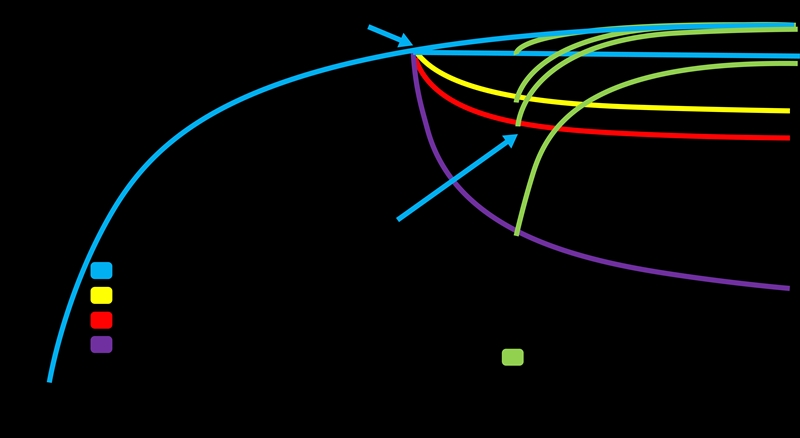
Rehabilitation professionals are faced with two problems when prescribing exercises. The first is the concept of ‘specificity.’ To regain tissue capacity, rehabilitation needs to expose tissues to sufficient stresses to induce adaptation. The ‘specific adaptation to imposed demands’ principle dictates that the body adapts to perform under the stresses it is exposed to regularly.Secondly, the concept of ‘reversibility’ is the ‘use it or lose it’ principle. Athletes start losing their training adaptations relatively rapidly when they stop training (see figure 1). For example, research has demonstrated that sprinting abilities begin to detrain within a week, while strength and aerobic fitness are affected after a month of detraining(1).
Figure 1 – The effect of detraining on physical fitness and the impact of various load maintenance strategies.
Injured individuals, therefore, suffer two significant consequences as a result of their injury:
- Acute pain and loss of function at the injury site.
- Gradual loss of general training adaptations.
Clinicians need to address both factors through the rehabilitation process. A critical choice that needs to be made early on in any rehabilitation process is maintaining or retraining. The timeline will influence this choice. For shorter-term injuries (< 3 months), it may be feasible to maintain the client’s physical conditioning by working around the injury site. However, it is often more practical to accept that a level of detraining will occur for longer-term injuries, and training volume and intensity must progressively increase as the function returns. In either case, athletes should attempt to avoid a complete withdrawal from all forms of training. Maintaining training exposure at as little as 30% of previous volumes reduces the return to full fitness time.
The programming puzzle
The most challenging aspect of exercise prescription is ensuring the correct training intensity. Even if clinicians get the mode, frequency, and volume prescription right, the training program won’t have the desired effect if the intensity is wrong. Therefore, training intensity and volumes should be as near an individual’s pre-injury loads as possible (see table 1).| Mode | Type of training - running, riding, strength training, etc. | ||
| Frequency | How often the client should train - prescribed as sessions per week. | ||
| Intensity | How hard to train - how much weight to lift or how fast to run. | ||
| Volume | The total amount of work required - prescribed as total distance, total time, or the number of sets, and reps. |
The most popular method of intensity prescription for exercise professionals is to base training on maximal capacities. To establish maximal capacities, clinicians may determine the maximum weight a client can lift for a particular movement, known as a 1-rep max (1RM). Clinicians will then prescribe training at a weight percentage, e.g., Squat 4 x 8 reps at 65% 1RM. Similarly, clinicians prescribe running intensity by determining an athlete’s best 1-mile time, e.g., 8 x 800m @ 115% of 1-mile speed.
The percentage-based approach to training prescription is common and widely accepted. However, it is subject to several problems that make it less than ideal in a rehabilitation setting.
- The use of this approach requires maximal capacity testing, which is usually not possible in injured clients. Furthermore, if an athlete completed maximal testing before their injury, capacity will likely be affected post-injury.
- Maximum capacity testing takes time, and it is usually impossible to test every exercise or modality in the program, so an element of guesswork persists.
- Changes in strength during the early phases of rehabilitation occur rapidly and are driven by increased muscle activation and neurological mechanisms, while the remodeling of muscles and tendons takes longer. Therefore, maximum capacity testing must take place frequently to account for these changes.
- Athletes experience day-to-day variability in their maximal capacities as these are affected by life stresses. For example, poor sleep and social pressures can affect an athlete’s training capacity. In addition, being unable to participate in regular training activities places psychological stress on clients so that percentage-based prescription can be particularly unreliable.
Autoregulation – the training prescription hack!
One plausible solution to the training prescription problems described above is the concept of autoregulation. Autoregulation is a training periodization approach that aims to adjust training prescription to the athlete’s daily capabilities(2). These adjustments ensure optimal training intensity. For example, clinicians reduce the intensity on days when the athlete is tired and maximize on days when they have the potential to push harder.There are strong and reliable relationships between the relative intensity of lifts (% of 1RM), the number of lifts that can be completed (repetitions in reserve- RIR), and the athlete’s perception of effort (rating of perceived exertion - RPE) during training(2). Therefore, prescribing training intensity using these alternative methods allows clinicians to create appropriate exercise programs without the need for 1 RM testing (see table 2). The significant advantage of using RIR and RPE to prescribe intensities is that the weights selected to reflect the athlete’s capacity on the day.
| Number of Repetitions | % of 1RM | Repetitions in Reserve (RIR) | Rating of Perceived Exertion (RPE) |
|---|---|---|---|
| 1 | 100 | Maximum Effort | 10 |
| 2 | 95 | No further reps, but could increase load | 9.5 |
| 3-4 | 90 | 1 | 9 |
| 5-6 | 85 | 1-2 | 8.5 |
| 7-8 | 80 | 2 | 8 |
| 9-10 | 75 | 2-3 | 7.5 |
| 11-12 | 70 | 3 | 7 |
| 12-15 | 65 | 4-6 reps remaining | 6.5 |
| 15-20 | 60 | 4-6 reps remaining | 6 |
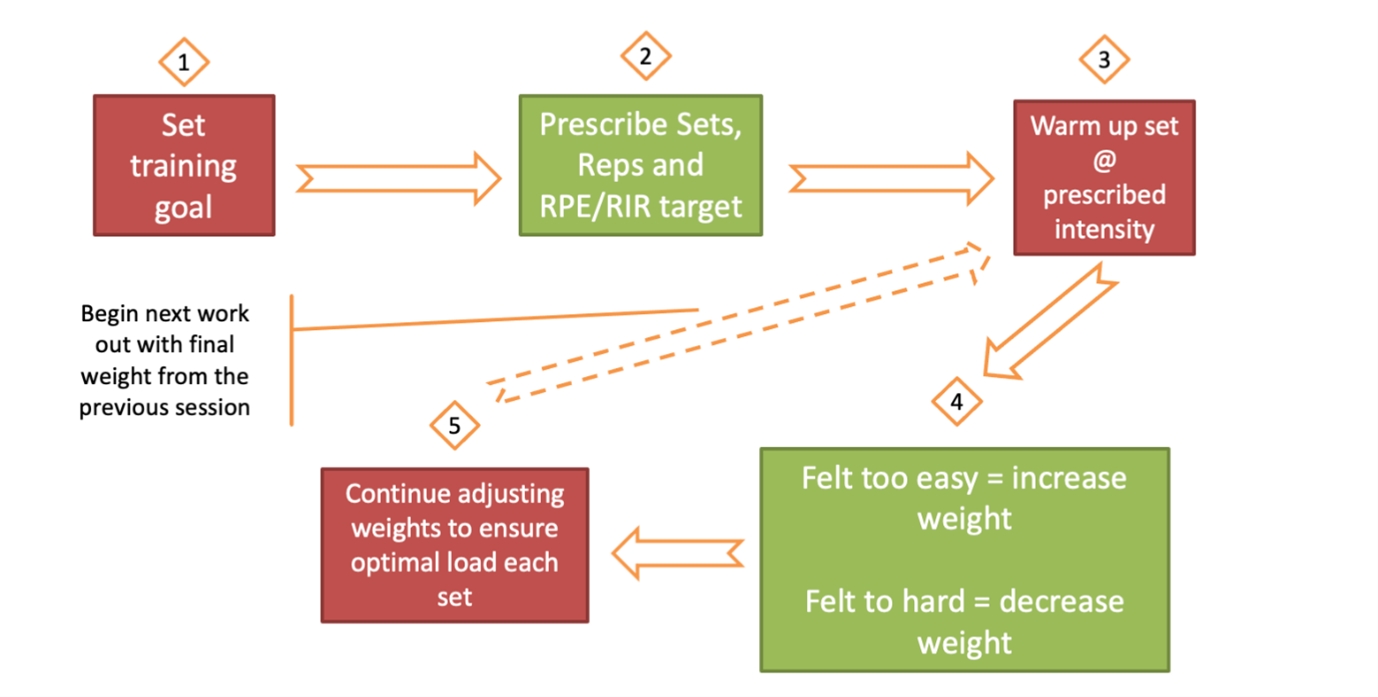
Autoregulation training prescription can be systematized to ensure progression over time. The critical steps are choosing a training goal, such as developing hypertrophy or maximal strength. There are published guidelines for intensity, set, and rep structures for these training goals. For example, an accepted approach for developing maximal strength is to complete four sets of five reps at an intensity of 85% 1RM. The athlete completes four sets of five reps at the perceived intensity of 8.5 out of 10, or with one to two RIR. After each set, the clinician asks the athlete, ‘How did that feel?’ If the actual intensity did not match the training prescription, i.e., the athlete felt like they didn’t have any RIR, the clinician adjusts the weight at the start of the next set. After the training session, the athlete records the finishing weights for all exercises, which become the starting points for the following session. Training continues in this manner, adjusting and optimizing load until the end of the training block when a new training goal is set (see figure 1).
Figure 1: The autoregulation approach to training
Conclusion
The autoregulation approach may seem overly simple, but it is highly effective. For example, researchers at the Auckland University of Technology demonstrated that prescribing training based on the perception of effort was marginally more effective than traditional percentage-based training(3). These findings should give rehabilitation professionals confidence that through applying the autoregulation approach, it is possible to optimally prescribe training intensities and avoid the associated detraining that rehabilitation periods have historically caused.References
- Block Periodization: Breakthrough in sports training. 2003
- J Strength Cond Res. 2020 Feb 13
- Front Physiol. 2018 Mar 21;9:247
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.






