You are viewing 1 of your 1 free articles
Sleeping sporting beauties: Part I - how hormones influence sleep
The role of sleep on performance is undeniable. However, female athletes’ sleep-recovery relationship may differ from their male counterparts due to their physiology. In part one, Candice MacMillan discusses how female hormones interact with the circadian rhythm and their impact on sleep.
Introduction
Sleep is a key element to peak athletic performance(1). It is regarded as one of the most effective recovery strategies and plays an integral role in the adaptive and recuperative processes(2). However, the recovery process is only optimal when sleep quantity and quality are adequate. High training volumes, competition demands, and exposure to numerous, ever-changing environmental factors may cause sleep impairments among elite-level athletes(3). Physiological factors unique to female athletes, such as fluctuating sex hormone levels throughout the menstrual cycle (MC), are additional culprits that influence the quality and quantity of sleep(4).
The female MC is superimposed on the circadian rhythm responsible for the sleep-wake cycle(5). Additionally, hormones related to physical and psychological stressors and those responsible for sexual maturation during adolescence can further amplify sleep impairment among female athletes. Thus, understanding female athletic development is critical to fully comprehend the cascade of possible collisions that could block the road to a peaceful night’s sleep.
Circadian rhythm and athlete stressor hormones
Numerous hormonal responses take place in the lead-up to and during sleep. Growth hormone (GH) is responsible for muscle growth, repair, and bone building. It is produced throughout the day, and 95% is released during non-rapid eye movement sleep (NREM)(2). Exercise is a physiological stressor that results in the release of cortisol and testosterone(3). While cortisol is a catabolic hormone, i.e., it stimulates the breakdown of molecules and energy production, testosterone is an anabolic hormone, i.e., stimulates growth and repair. The balance and timing of these hormones are essential for muscle adaptation, growth, and restoration. Growth hormone, cortisol, and testosterone follow the circadian rhythm. Sleep deprivation results in increased cortisol levels and affects the secretion pattern of testosterone and GH, ultimately disturbing the anabolic-catabolic patterns(2,3). During sleep debt, the shift in catabolic hormones contributes to muscle mass loss and reduced muscle recovery(4). In response to exercise and sleep deprivation, the fluctuations in hormonal profiles differ between athletes and non-athletes at rest.
The secretion of melatonin initiates sleep through the synchronization of environmental cues, and is suppressed by exercise(5). The consequence of exercise on melatonin varies depending on the timing, length, and intensity of training sessions(2,5). The secretion and timing of melatonin and cortisol release are inversely proportionate(6). Melatonin levels are high during the biological night when cortisol levels are minimal. The opposing effects of vigorous exercise on melatonin and cortisol secretion may lead to sleep impairments among elite-level athletes (see figure 1)(2,6).
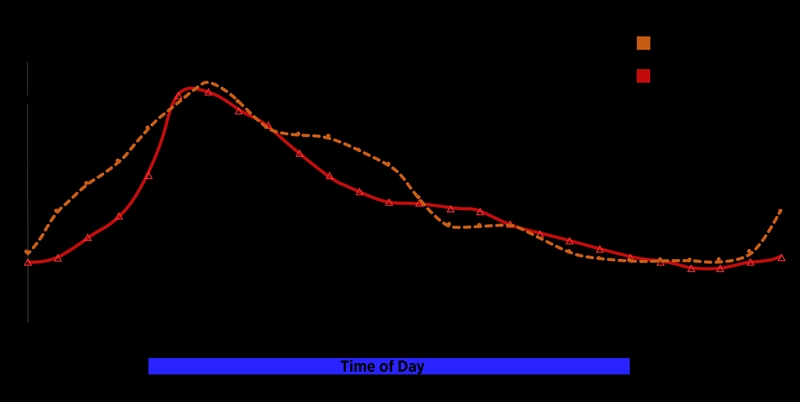
Figure 1: The 24-hour circadian cycle release of cortisol, testosterone, and melatonin
There is conflicting evidence of the effect of the MC on both melatonin and cortisol in females(5). While some evidence demonstrates no difference in melatonin levels during the luteal phase (LP) and follicular phase (FP), other researchers have found that total 24-hour melatonin secretion was significantly less during the LP than the FP. In addition, the understanding of the effect of the MC on cortisol secretion is limited.
The menstrual cycle-sleep relationship
Researchers at the McGill University in Montreal found objective sleep data indicates that females have more optimal sleep in less time awake during the night, longer sleep duration, shorter sleep latency, and greater sleep efficiency than male athletes(7). However, contradictory subjective data indicates higher incidences of poor sleep among females(5,7,8). There does appear to be a relationship between menstrual hormonal fluctuations and sleep impairments(3,5,8). The MC phases affect the circadian rhythm in temperature, selected hormone profiles, and sleep-wake behavior(5,8). This is due to the cyclic fluctuations of reproductive hormones that occur during a regular ovulatory MC.
Sleep impairments also occur due to symptoms associated with menstruation, including cramps, bloating, joint ache, painful breasts, anxiety, and mood changes(4,7). In addition, fluctuating hormone levels alter females’ sleep architecture. The hormones responsible for the MC include luteinizing hormone (LH), follicle-stimulating hormone (FSH), estrogen, and progesterone (see figure 2)(6).

Figure 2: The menstrual cycle and hormonal fluctuations*
*Adapted from a graphic created by Dr. Laura Bowen, lead women’s and girls’ sports scientist at Southampton FC. Used with permission from Women’s Soccer Coaching. 2021 Feb;03:9.
The LH and FSH regulate the secretion of estrogen. Progesterone has sleep-promoting effects during the early luteal phase, and females report feeling more lethargic throughout the day. As progesterone levels decrease at the end of the luteal phase, sleep may be disturbed(5,7,8). Estrogen also promotes sleep. Therefore, most females report difficulty sleeping just before and at the start of menstruation when estrogen levels are lower.

Figure 3: Hormonal fluctuation and related temperature changes during a typical MC(9).
Body temperature is associated with the onset and quality of sleep (see figure 3). Progesterone is responsible for the increase in body temperature(5). In contrast, estrogen secretion lowers body temperature. One possible explanation for the reduced amplitude in body temperature is the progesterone-mediated inhibition of the hypothermic action of melatonin in the LP. However, the increased progesterone estrogen ratio during the LP is responsible for the decline in the rate of nocturnal body temperature drop, rather than the isolated effect of increased progesterone (see table 1)(8).
Table 1: Summary of the menstrual hormonal fluctuations and effects on sleep.
| Menstrual phase | Hormone secretion | Effect on sleep |
|---|---|---|
| Follicular phase | Low estrogen and progesterone levels | High reports of poor-quality sleep |
| Luteal phase | A sudden drop in progesterone and estrogen levels | Poor sleep quality three days before menstruation and end of LP |
Oral contraceptives
Many female athletes use various methods of contraception to alleviate symptoms of natural menstruation and regulate their cycles to coincide with training and competition schedules. However, contraceptives suppress natural reproductive hormones, thereby preventing ovulation and natural MCs. In addition, oral contraceptives alter temperature, melatonin rhythms, and sleep architecture(5,8).
The effect of oral contraceptives on sleep
- Increased body temperature (thermogenic effect of progestins included in contraceptives)
- Increased nocturnal melatonin levels
- Decreased slow-wave sleep
- Shorter rapid eye movement (REM) sleep latency
- Greater REM sleep duration
Adolescent females
Adolescent females are at particular risk of sleep impairments during development. However, there is limited evidence to understand the relationship between sleep and menstruation in prepubertal and young adolescent female athletes(4). After their first menstrual bleed, females are 2.75 times more likely to develop sleep impairments than age-matched males(7).
Researchers at the Norwegian University of Science and Technology found that late adolescent female endurance athletes report longer times in bed, deep sleep, and shorter light sleep during menstrual bleeding than non-bleeding days. Furthermore, during the FP, athletes experience lower sleep efficiency and more deep sleep than the LP(7). Poor quality sleep among female youth athletes is related to developmental consequences such as delayed puberty and amenorrhea. In addition, possible long-term consequences include the female athlete triad, i.e., decreased energy, irregular menses, and reduced bone density(4).
Clinical implications
The cumulative effects of menstrual and athletic stressor hormones, superimposed on the natural circadian rhythm, predispose female athletes to sleep impairments. Clinicians need to understand how high energy demands related to sport affect sleep and maturation among prepubertal and young female athletes. The effect of sleep impairments and hormonal imbalance may result in developmental delays and increase the risk for the female athlete triad.
To reduce the impact of changes in hormones throughout the MC, clinicians and athletes need to better understand the athlete’s sleep at different stages of the cycle. Clinicians may advise the use of a sleep diary in athletes with sleep disturbance and decreased performance. Athletes will require an individualized management strategy as not all athletes experience sleep disturbance during their MC. The manipulation of training loads, recovery strategies, and referral to appropriate medical professionals will assist in the holistic management of athletes.
References
- British J of Sports Med. 2019;53(8):513-522.
- NSS. 2018;Volume 10:243-253.
- Euro J of Sport Sci. 2018;18(5):611-618.
- Sports Med - Open. 2021;7(1):57.
- Sleep Med. 2007;8(6):613-622.
- Int J of Endo. 2010;2010:1-17.
- PLoS ONE. 2021;16(6):e0253376.
- Sleep Med Clin. 2018;13(3):283-294.
- Am J Respir Crit Care Med. 2013;187(4):366-373.
Related Files
Further reading
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









