Eyes-up: sensorimotor integration issues post whiplash-associated disorders
Sensorimotor integration is often affected following traumatic head and neck injuries. However, the signs and symptoms are not always obvious. In sports, the smallest deficits can increase injury risk and impair performance. Megyn Robertson explores the assessment of sensorimotor integration to improve clinical outcomes following WAD.

New Orleans Saints wide receiver Taysom Hill suffers an apparent neck injury against the Washington Football Team during the first half at FedExField. Mandatory Credit: Brad Mills-USA TODAY Sports
Athletes who sustain whiplash-associated disorders (WAD) are at risk of developing sensorimotor incongruence. This may be the reason why they experience persistent head and neck pain. In addition, athletes may report subtle unsteadiness or dizziness, lightheadedness, visual disturbances (e.g., blurry vision), difficulty reading, motion sickness, changes in cervical proprioception, head and eye movement control, and changes in postural stability(1). While the figures vary depending on the cohort studied, up to 50% of people who experience a whiplash injury will never fully recover, and up to 30% will remain moderately to severely disabled by their condition(2). Furthermore, the associated costs secondary to whiplash injury, including medical care, disability, lost work productivity, and personal costs, are substantial(3).
Understanding these signs and symptoms is important to effectively assess and treat this patient population. Clinicians should be suspicious of red flags and differential diagnoses, such as vertebral basilar insufficiency (VBI) or psychosocial factors, such as anxiety or fear avoidance behaviors in these traumatic neck pain patients(4). The combination of dizziness and neck pain does not necessarily indicate the neck is the source of dizziness. The Postural Control System plays an integral role in the human body, it ensures that we can remain upright against gravity (postural equilibrium) and holds our head and neck in an advantageous position such that we get maximal input from our five senses (postural orientation), which ultimately protects us against potential threat or injury from the external environment.
The upper cervical spine is a highly developed proprioceptive system of mechanoreceptors. It provides afferent input for superior neuromuscular performance and direct neurophysiological connections with the vestibular and visual systems(1,5). However, the upper cervical spine is a significantly mobile segment which makes it vulnerable, especially if trauma is involved, as in a whiplash or concussive disorder.
What is sensorimotor integration?
Sensorimotor integration is the coordination of the cervical somatosensory, visual and vestibular input, which allows the brain stem to determine the position of your head in space. The sensorimotor system utilizes several reflexes to influence head orientation, postural stability, and eye movement control, namely, the vestibular ocular reflex, vestibular spinal reflex, tonic neck reflex, cervicocollic reflex, and the vestibulocollic reflex (see table 1).
Table 1: Sensorimotor system reflex functions(4,6)
| Reflex | Function |
|---|---|
| Vestibular ocular | Maintains clear vision (gaze stability) while the head moves |
| Vestibular spinal | Vestibular spinal and tonic neck reflexes work together to maintain an upright head position while the body or lower extremity is engaged in other active movements |
| Tonic neck | |
| Cervicocollic | Cervicocollic and vestibulocollic reflexes work together to prevent excessive neck rotation |
| Vestibulocollic |
Sometimes after a WAD or head trauma, there is a sensory deficit due to altered cervical afferent input. This may result from inflammation (chemical changes) affecting receptor sensitivity. Altered sensory input leads to poor central integration and processing components, resulting in a mismatch in efferent output, which affects the integration, timing, and tuning of sensorimotor control(6). This makes it challenging to maintain stability in the postural control system.
Rehabilitation specialists aim to prevent athletes from developing chronic neck pain. There are three systems that clinicians should prioritize in the assessment, namely proprioception, eye movement control, and balance(5). Once properly assessed, clinicians can implement appropriate patient-specific management.
Sensorimotor integration assessment?
Proprioception
Joint position sense (JPS) is the ability to relocate the natural head position without the assistance of visual input. To assess JPS, the patient sits 90cm away from a visual target with a laser pointer attached to a headband. At the start, the patient centers the laser on the target. Then, they close their eyes, rotate their head to the left, and return to the midline. The patient can then open their eyes and see how close they are to their original head position. The test is repeated to the right and again into flexion and extension. The clinicians measure the distance from the target for three attempts in each direction. If the patient’s laser pinpoint sits further than 6.5cm from the center of the target, then the test is positive for poor JPS. If the laser falls between 3-5cm from the center of the target, it’s considered normal (see figure 1). Other positive tests include poor motor control of their head and neck in various positions, or the patient reports feelings of dizziness or unsteadiness when performing the test(7).
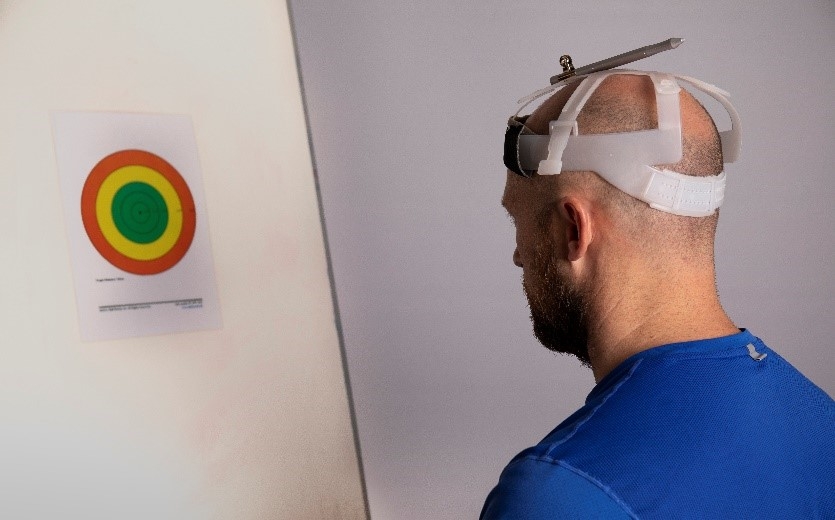 Figure 1: Assessing joint position sense
Figure 1: Assessing joint position sense
Eye movement control
- Gaze stability is the ability of the eyes to fixate on a stable point when the head is moving in space.
- Smooth pursuit is the ability of the eyes to follow a slowly moving object smoothly. With the head and trunk in neutral, the patient’s eye movement control is tested by following a slow figure of eight. A positive test is if the patient displays any saccadic eye movement or complains of feeling dizzy or unsteady(5).
- Smooth Pursuit Neck Torsion Test (SPNTT) differentiates between vestibular pathology and cervical afferent dysfunction due to neck pain and is a progression of the Smooth Pursuit test. The patient’s trunk is rotated 45 degrees in either direction while the head remains in neutral. The patient’s eye movement control is tested by following a slow figure of eight (see figure 2). A positive test means that there is a change in eye movement control or becomes saccadic when the trunk rotates to one of the sides. Poor eye movement control with trunk rotation to both sides is more likely a central nervous system disorder and not sensorimotor impairment(8).
 Figure 2: Assessing gaze stability
Figure 2: Assessing gaze stability
Balance
Neck fatigue following WAD is related to balance disturbances. The Balance Error Scoring System (BESS) test provides a portable, cost-effective, and objective method of assessing static postural stability. Athletes perform the test in three positions - bilateral stance, tandem, and single leg stance on a stable and unstable surface (Airex foam mat) (see figure 3). The BESS tests are performed with the eyes open and then closed for 20 seconds in each test position. Each time the patient steps, stumbles, or falls, opens their eyes, remains out of the test position for more than 5 seconds, sways, abducts, or flexes their hip more than 30°, or lifts their foot off of the testing surface, the clinician adds a point. If the patient attains 10 points for any single balance stance, this is a positive test for balance impairment(9).

Figure 3: The Balance Error Scoring System (BESS) test
Translating research into clinical practice?
The assessment of an athlete’s sensorimotor integration is essential following a WAD. The tests that bring on the patient’s symptoms identify the required treatment protocol. Given the close physiological connections and adaptations involved in the sensorimotor control system, managing these disturbances is likely to be multimodal. It may mean addressing the primary causes and secondary adaptive changes in the sensorimotor control system.
In conclusion, a patient-specific sensorimotor approach with exercises to improve the identified deficits in cervical joint position and movement sense, oculomotor function, and static and dynamic balance are essential for any WAD rehabilitation program(1). Therefore, clinicians should assess sensorimotor integration early following head and neck trauma, irrespective of if athletes present with symptoms. Clinicians are urged to do further reading to enhance their understanding and improve clinical outcomes.
References
- JOSPT 2017 Jul;47(7):492-502.
- Pain 2006;122:102–8
- J Man Manip Ther. 2011 Nov; 19(4): 194–200.
- 2009 May;39(5):364-77.
- www.chrisworsfold.com/eye-movement-control-in-neck-pain/
- Manual therapy. 2008 Feb 1;13(1):2-11.
- J of Ortho Research 25(3): 404-412.
- Otology & Neurotology 19(1): 76.
- www.apta.org/patient-care/evidence-based-practice-resources/test-measures/balance-error-scoring-system-bess#
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










