Masterclass: Femoro-acetabular impingement (FAI) - Part I
In the first part of this two-part article, Chris Mallac looks at the surgery and rehab options for Femoroacetabular impingement (FAI), an increasingly common musculoskeletal disorder that can affect young to middle-aged athletes. In part two, Chris will describe in detail the post-operative rehabilitation period required to take an athlete back to full competition.

2018 Rotherham United’s Ryan Williams in action with Scunthorpe United’s Rory McArdle Action Images/Ed Sykes
Introduction
The idea that abnormal hip morphology was a possible cause of hip degeneration and arthritis was initially suggested by Stulberg et al (1975), when they identified the ‘pistol grip deformity’ in the x-ray findings of abnormal head of the femur (HOF) clearance from the acetabulum in patients with hip arthritis(1). This led to the idea that mechanical impingement may be one of the underlying causes of hip degeneration and hip joint pain.
Over the next few decades, with improvements in radiology and hip joint surgery, and more sophisticated clinical assessment skills, it was recognized that a number of atypical hip joint morphologies commonly existed that may give rise to hip joint pain in athletes.
In the late 1990s, Mayer et al (1999) were the first to use the term ‘Femoroacetabular impingement’ or ‘FAI’ to describe the morphology of the hip as being a causative factor in hip joint arthritis, and the concept of FAI was further pioneered by Reinhold and colleagues during the early 2000s(2,3).
An FAI is a genuine complication for an athlete, particularly for young male athletes, as it can not only lead to hip joint pain and labral and cartilage damage, but it can also give rise to other athletic injuries such as osteitis pubis and inguinal hernias due to the detrimental effect that a lack of hip joint rotation plays on pelvis stress injuries(4).
The purpose of this Rehabilitation Masterclass is to explain the relevant anatomy and biomechanics of the hip joint, explain the pathogenesis of FAI, offer management ideas, and an in-depth overview of the rehabilitation of the hip joint post-FAI surgery.
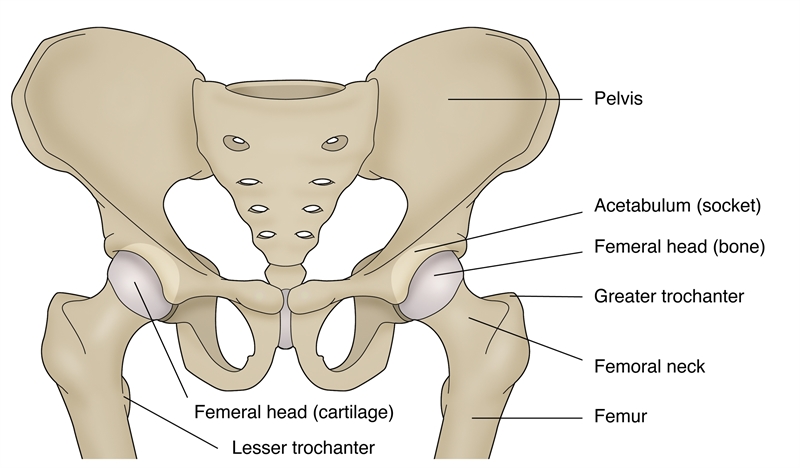 Figure 1: Hip anatomy
Figure 1: Hip anatomy
Relevant anatomy and biomechanics
The hip joint is a ball and socket joint that enjoys a wide range of movement into all planes of motion. It can also accommodate a large weight-bearing force during locomotion (see figure 1). The ‘normal’ hip morphology is identified as(5);
- The femoral head is slightly more than half a sphere.
- The femoral neck is cylindrical, narrowest in the midpoint and widest laterally, and attaches the head to the shaft.
- The acetabulum is cup-shaped.
- The labrum is triangular in cross-section, with its base attached to the acetabular rim.
Usually, a space is maintained between the femoral head-neck junction and the acetabular rim, and this provides unhindered hip movement. This is achieved with an offset between the anterior and superior surface of the femoral neck and the corresponding surface of the femoral head. The normal head-neck offset is 9mm(6).
Symptoms
Abnormal morphology of the hip joint can lead to impingement-type symptoms. A deviation away from the normal alignment of the hip can lead to a mechanical blockage between the acetabular rim and/ or head-neck of the femur. This deviation away from the normal may be due to inherent geometry faults in the patient’s hip joint complex. Inherent factors that may predispose to impingement are(5):
- Pistol grip deformity of the femoral neck (see figure 2).
- Reduced femoral neck offset in the anterolateral aspect of head neck junction (see figure 3).
- Reduced femoral anteversion (see figure 4).
Other factors include:
- Loss of sphericity in the femoral head.
- Excessive coverage of acetabulum
- Retroversion of acetabulum (causes over-coverage and restricts flexion of the femoral neck).
- Coxa profunda deformity floor of the acetabulum touches the ilio-ischial line) increases the depth of the acetabulum.
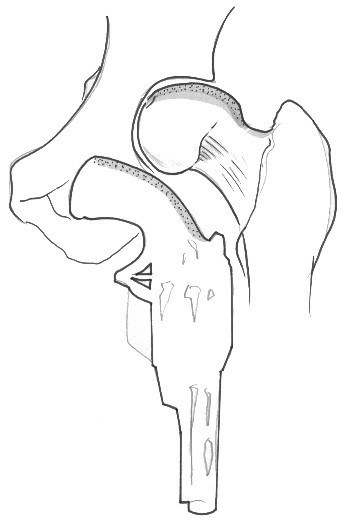
Figure 2: Pistol grip deformity of the femoral neck
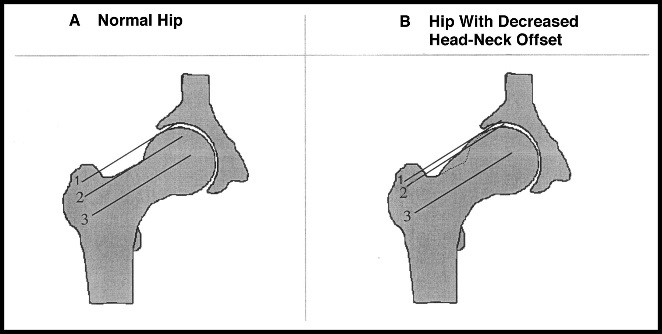
Figure 3: Reduced femoral neck offset in the anterolateral aspect of head-neck junction
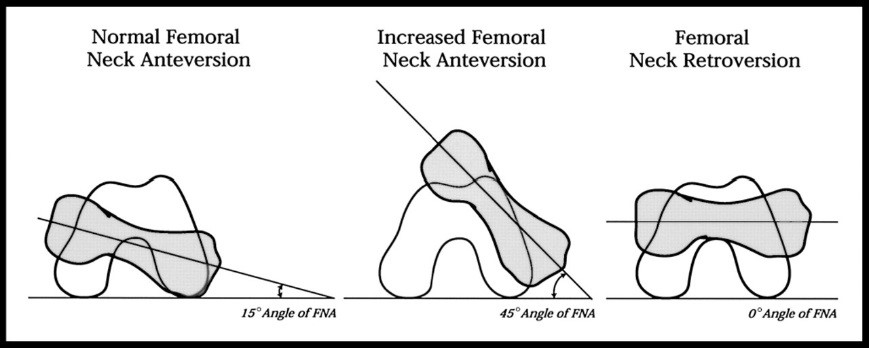
Figure 4: Reduced femoral anteversion
FAI as an injury
Although some examples of hip joint impingement are caused by inherent hip joint abnormalities, FAI as an injury is an anatomical mal-alignment between the head and neck of the femur and the acetabulum. This causes compression of the labrum and articular cartilage during hip flexion, manifesting as anterior hip pain and progression to early osteoarthritis of the hip. It is a condition that seems to affect younger, more active people, particularly males. For example, in a radiological study of 155 young active patients 18-50 years of age with complaints of hip pain, it was found that a staggering 87% of subjects had evidence of an FAI(7).
The natural progression of an FAI to full-blown hip joint disease has been postulated by McCarthy et al (2001)(8). They propose that initially, an FAI causes excessive loads on the acetabular labrum at extreme ranges of movement. As the labrum frays along the articular margins, this progresses to a more consequential tear of the labrum. The articular cartilage then delaminates away from the articular margin adjacent to the labral lesion. This then leads to abnormal shear forces across the joint, which over the long term, causes more global labral and articular degeneration.
Furthermore, more recent research suggests a strong link between FAI and other athletic groin pain syndromes, in particular athletic pubalgia. Economopoulos et al (2014) found that in 43 patients who underwent surgery for athletic pubalgia, 86% of them had evidence of an FAI in at least one hip, with Cam lesions being the most prevalent (see below for Cam lesion)(9). This highlights the possible interaction between forces acting across the pelvis and hip joint. Hammoud et al (2014) provides an in-depth discussion on how an FAI can possibly lead to mechanical compensation patterns, which can, in turn, lead to a host of sports injuries such as osteitis pubis, sacroiliac joint problems, posterior hip impingement, and proximal hamstring syndrome just to name a few(10). In the context of FAI, two main manifestations of FAI have been described. These are ‘Cam’ and ‘Pincer’ lesions (see figure 5).
Cam lesions
The Cam lesion is attributed to an asymmetric or nonspherical portion of the femoral head or neck abutting against an acetabular rim. This abutment is most evident in flexion and internal rotation, where a shear force occurs along the anterolateral edge of the acetabulum. This deformity decreases the head-neck offset, increases the femoral head radius of curvature, and results in relative retroversion of the femoral head.
The smooth motion between the femoral head and acetabulum is lost, which causes an outside-in abrasion of the acetabular cartilage with avulsion from the labrum and subchondral bone (delamination). This can lead to the separation of the cartilage from the anterosuperior aspect of the labrum(11). Labral injuries are more likely to affect the anterior region, possibly due to its poor blood supply. Also, it is a mechanically weaker area of the labrum, and the anterior labrum experiences more loads and shear than other areas of the labrum(12).
Cam lesions are common in young active men, with a ratio of around 25% in asymptomatic hips and up to 78% in symptomatic hips(13,14). It is more prevalent in men than in women at a ratio of 3:1(15). It is possible that a major factor in the development of a Cam lesion is a slipped capital femoral epiphysis where posterior displacement of the capitis leaves a prominence of the anterior neck, resulting in severely limited internal rotation of the hip(16). Furthermore, pistol grip deformities can lead to more subtle forms of aspherical femur heads, and these have been associated with early-onset osteoarthritis in adults.
| Causes of Cam Lesions |
|---|
|
1. Idiopathic 2. Developmental (Non-spherical femoral head, Coxa vara) 3. Traumatic (malunited femoral neck fracture; post-traumatic retro version of the femoral head 4. Childhood orthopedic conditions (Perthes disease; slipped capital femoral epiphysis) 5. Iatrogenic (femoral osteotomy) |
Pincer lesions
Pincer lesions create repeated contact between a normal femoral head-neck junction and an over-covered acetabular rim. This results in multiple cleavage planes in the labrum and subsequent labral degeneration, intrasubstance ganglion formation, ossification of the acetabular rim, and ultimately a deepening of the acetabulum, further compounding the pincer lesion.
Unlike in cam lesions, the chondral damage associated with pincer lesions is more circumferential at the anterior and superolateral acetabular rim, where force transmission is larger and as a ‘contrecoup’ lesion in the posterior capsular labral junction due to the ‘levering’ out the femoral head along the fulcrum created by the anterior pincer lesion whilst the hip is flexing(17).
Retroversion of the pelvis can also cause the acetabular rim to roll backward. It is to be noted that spinal deformities like scoliosis or kyphosis can cause pelvic rotation and functional retroversion of the acetabulum, which may act as a pincer lesion. There can also be an extra bit of bone along the anterior rim of the acetabulum, known as an ‘os acetabulum’(18). Pincer lesions are more common in active females(19).
| Causes of Pincer Lesions |
|---|
|
1. Idiopathic 2. Developmental (retroverted acetabulum; Coxa profunda; os acetabuli; protrusio acetabuli; chronic residual dysplasia of the acetabulum) 3. Traumatic (post-traumatic deformity of the acetabulum) 4. Latrogenic (over-correction of retroversion in dysplastic hips) |
Mixed lesions
Rarely do cam and pincer lesions occur in isolation. Most type of FAI occurs from the mixed cam and pincer pathology at the anterior femoral neck and anterior superior acetabular rim. However, Cobb et al. (2010) argued against this after analyzing the morphology of 60 acetabula with CT scans(20). They reported that acetabula with cam hips were shallower than normal hips, which in turn were shallower than pincer hips. Hence, they concluded that cam and pincer lesions were different pathoanatomic entities, with cam hips being shallow while the pincer hips are deeper than normal hips.
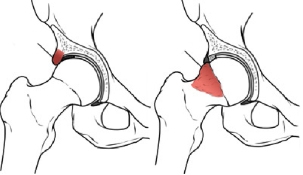
Figure 5: Cam and pincer lesions
Signs and symptoms of FAI
FAI in the athlete may present as insidious onset groin pain worsened by hip flexion and hip flexion with internal rotation-type movements. It is more common in male athletes due to the male predisposition towards Cam impingements. Sports with a higher incidence of FAI are sports that involve a lot of forced flexion with internal rotation, such as treading water in water polo, breaststroke kicking, football sports such as soccer and AFL, rugby, field hockey, combat sports such as wrestling and Brazilian Jujitsu and ice hockey.
The athlete themselves may aid the diagnosis by offering information regarding childhood diseases that can lead to abnormal head and neck junctions. Conditions such as Perthes disease (3-12-year-olds) or slipped capital femoral epiphysis (SCFE) (12-14-year-olds) may alert the sports medicine practitioner that an underlying FAI may be present.
- The typical collection of signs and symptoms are; Insidious onset of symptoms in active young and middle-aged adults.
- Groin pain associated with activity and no prior history of trauma.
- Inability to perform activities such as high hip flexion or prolonged sitting.
- It may hurt moving from sitting or squatting to standing.
- Sharp stabbing pain with movements such as aggressive turning or pivoting.
- Painful clicking, locking, or instability from a labral tear secondary to undiagnosed FAI.
- Reduced range of motion, especially flexion, adduction, and internal rotation. Often athletes notice that they are not as flexible as their teammates.
Objective signs
Due to inherent hip muscle weakness associated with the hip joint pathology, the patient may often show poor proximal pelvic control during single stance tests, and a Trendelenburg sign may be present. Passive range of motion will be limited compared with the non-affected side, particularly hip flexion (usually less than 110°) and hip internal rotation (less than 15°). A number of tests have been proposed that may assist the sports medicine practitioner in clinically identifying an FAI in an athlete.
Impingement tests
FADDIR sign– This test involves passive hip joint flexion, adduction and internal rotation (Flexion-ADDuction- Internal Rotation)(21). Pain is felt deep in the anterior hip/groin area, and the assessor may feel a mechanical block to movement (see figure 6).
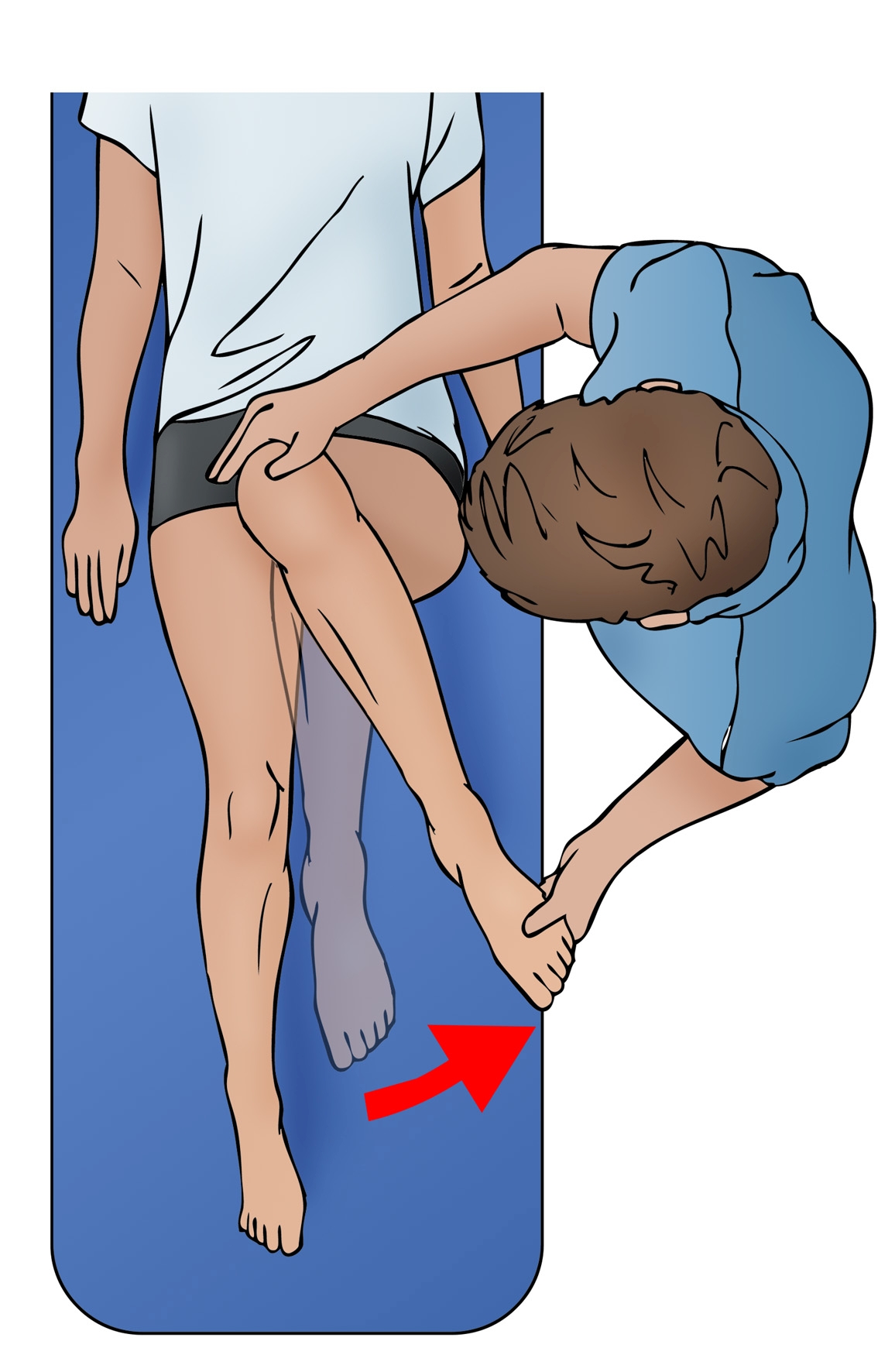
Figure 6: FADDIR test
Posterior inferior impingement test – With the hip in hyperextension, passively hanging the leg over the end of the bed, the affected hip is passively externally rotated(22). The test is positive if it elicits similar pain as complained by the patient.
FABER test – With the hip in flexion, abduction and external rotation (Flexion- ABDuction, External Rotation), abutment of the labrum and cartilage also can occur (see figure 7)(23). The test is positive if it elicits similar pain as complained of by the patient or if the distance between the lateral knee and the exam table differs between the symptomatic and contralateral hip.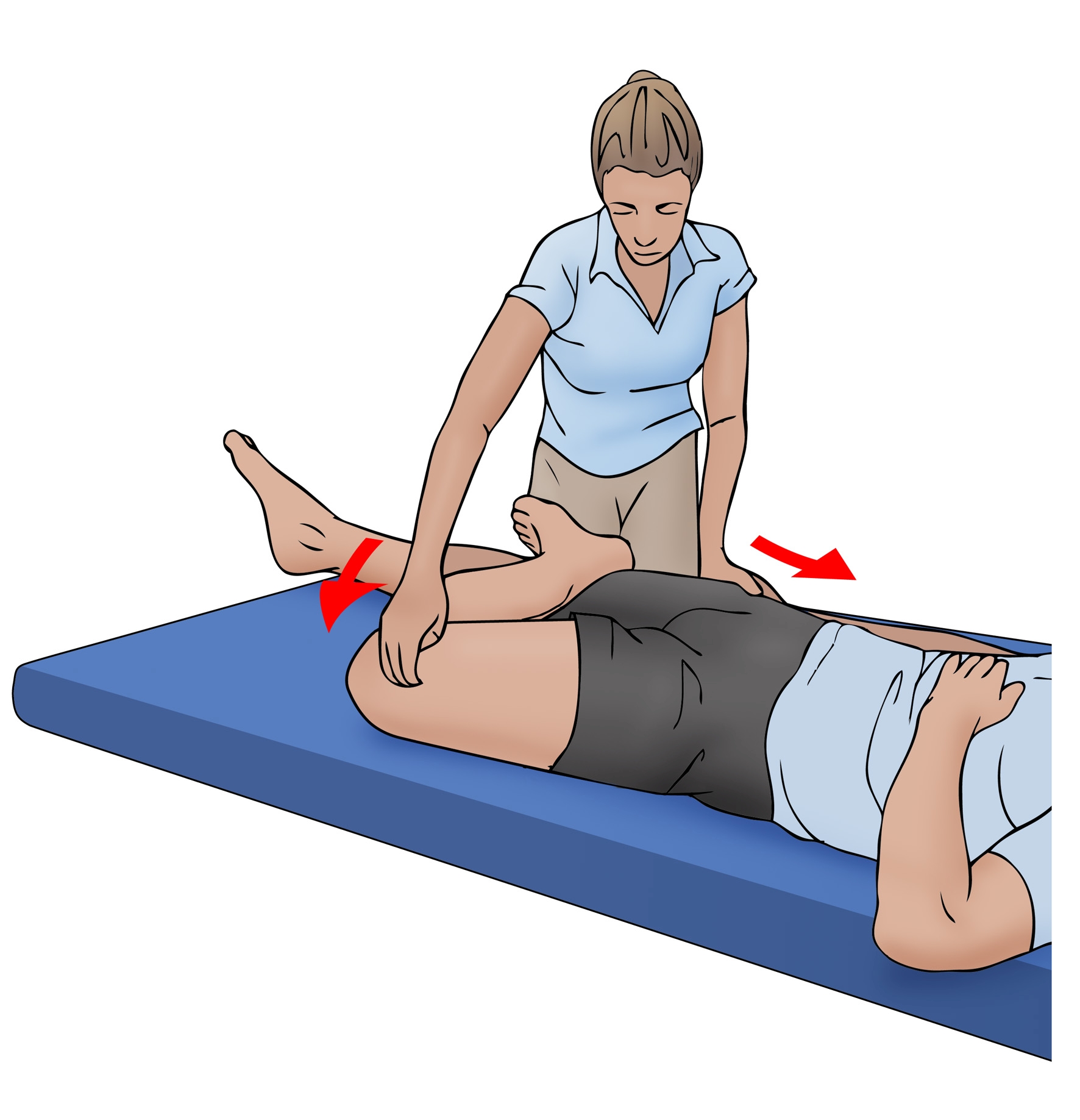
Figure 7: FABER test
Radiographs
Anterior/posterior (AP) views
Well-centered AP views are necessary to view Cam lesions (due to flattened head-neck junction, pistol grip deformity), any degenerative hip joint changes (sclerosis, osteophytes, reduced joint space), and a profunda socket. AP views will also define the acetabular version, such as the crossover sign. This may also be seen as indicative of a prominent anterior acetabular wall (pincer impingement). Anteroposterior views will show acetabular retroversion, acetabular depth, os acetabulum, and/or herniation pit in the neck of the femur, and/or impingement cysts may be present.
Standard Lateral view
This will identify subchondral bone sclerosis and cyst formation of the anterior acetabular rim.
Cross table lateral views/frog lateral views
This can be done in 10-15° internal hip rotation to compensate for femoral anteversion. This is best to view the Cam impingement lesion and reactive fibro cystic changes of the anterior head-neck junction. Other radiological measurements that can be made include head-neck offset, alpha angles, and anterior offset ratio(24.25.26).
Magnetic resonance imaging (MRI) and arthrography (MRA)
Magnetic Resonance Imaging is useful if hip labral pathology is suspected in conjunction with FAI and may show articular cartilage thinning. Increased signal on T2-weighted images in the anterior acetabulum may be indicative of subchondral edema, which may be incorrectly interpreted as a stress fracture of the anterior inferior iliac spine. It is more likely indicative of a subchondral stress reaction in the anterior acetabulum due to failure of the subjacent articular surface. Thus, anterior acetabular subchondral edema is suggestive of significant articular pathology(27).
Magnetic Resonance Arthrography is much more sensitive for viewing intra-articular pathology, including labral lesions. This can also be useful, as the gadolinium injection associated with the MRA also has a local anesthetic that can be used as a diagnostic block for intra-articular joint pathology.
Computerized tomography (CT)
Computerized tomography 3D reconstructions are useful to assess the shape of the femoral head-neck junction, and this is considered useful for surgical resection. A new CT view has been developed by Pritchard and O’Donnell to demonstrate FAI lesions CT scanning in the position of discomfort (POD view) allows symptomatic Cam deformity to be accurately mapped in a 3-dimensional reconstruction (see figure 8)(28). This procedure helps in the diagnosis of the problem by visualization and subsequent planning for surgical resection.

Figure 8: A 3-dimensional reconstruction of Cam lesion
Surgery
Due to the mechanical nature of FAI, conservative management along with physiotherapy usually fails as, ultimately, the osseous impingement restricts the athlete. Often conservative programs are only effective in acting as identifiers of FAI and then preventing further mechanical symptoms by avoiding the offending movements. Gym-based movements such as squats past 60° hip flexion, Bulgarian squats, and leg press are avoided or modified to be performed in external rotation. However, ultimately if pain persists, then surgery is the only way to manage these problems.
Prior to the development of more advanced hip joint surgery techniques, athletes with ‘FAI’ would have lived and performed within the confines of their symptoms. They simply would have avoided movements that created hip joint pain, and if this proved too difficult to avoid, they simply would have ceased to compete.
In this current day, advancements in not only diagnosis but also both open and arthroscopic hip joint surgery have allowed simple management of these conditions. Therefore surgery is often recommended for the young athlete with FAI. The purpose of surgery is to remove the mechanical block of the proximal femur against the acetabulum and to also address any associated labral pathology and articular damage. Open and closed arthroscopic techniques have been described.
Before 2001, direct access into the hip joint was very difficult due to the risk of avascular necrosis. Therefore most hip joint impingements were managed with labral debridement and/or labral reattachment. In 2001, Ganz et al described a surgical technique that involved surgical dislocation with a ‘trochanteric flip osteotomy’ that preserved the blood flow to the femoral head(29). This avoided the serious side effect of avascular necrosis of the femoral head associated with hip joint dislocation procedures. This technique led to better identification of FAI as a genuine hip joint pathology, and correcting this surgically was now possible.
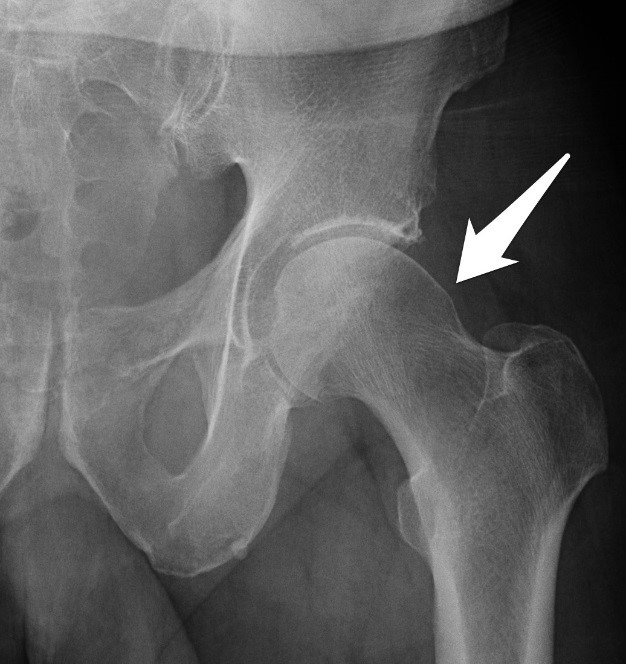
Figure 9: AP xray showing a prominent femoral neck
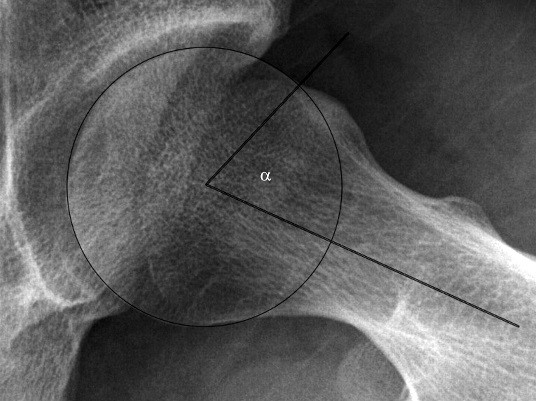
Figure 10: Alpha angle of the head neck of femur
Open surgery
This involves the dislocation of the hip anteriorly using a trochanteric flap osteotomy. This allows a full view of the head-neck junction. Any osseous impingement visualized can then be excised to restore the normal contour of the femoral neck junction. Retroversion of the acetabulum can be managed with resection of the prominent anterior acetabular rim. Any labral tear should be treated with excision or repair.
Ongoing groin pain following an open procedure can be caused by the insufficient restoration of the femoral or acetabular morphology, advanced joint degeneration, joint space narrowing, ongoing cartilage damage, or scar adhesions between the hip joint capsule and femoral neck resection, and between the labrum and hip joint capsule. If this scarring is thick, then it may interfere with movement between the femur and the acetabulum. These can impinge during flexion and internal rotation movements.
Arthroscopic repair
Arthroscopic intervention is now becoming increasingly popular. Two areas can be examined under arthroscopy(30);
- Central compartment – the structures medial to the labrum.
- Peripheral compartment – the structures outside the labrum but inside the hip capsule.
The arthroscopic procedure is performed with the patient lying supine or lateral decubitus. A traction device is used to separate the femur from the acetabulum to visualize the central compartment. Traction is not needed for peripheral compartment procedures. The joint is filled with saline, and two to three portals are used (anterior, anterolateral, and/or posterolateral).
The procedures achieved by hip arthroscopy at present include;
- Debridement of labral tear
- Repair of a torn labrum
- Chondroplasty of acetabular lesions
- Drilling or microfracture of acetabular lesions
- Acetabular rim excision (pincer lesions)
- Debridement of acetabular chondral delamination
- Capsular excision
- Femoral osteochondroplasty
Philippon et al (2007) found that 93% of athletes returned to competitive sports following arthroscopically managed FAI(31). The small number who did not have advanced OA changes at the time of surgery. Conclusion FAI is an increasingly more common musculoskeletal disorder affecting young to middle-aged athletes that can lead to insidious onset groin pain and damage the hip joint labrum, and lead to early OA changes. It is common in sports that require hip flexion and hip rotation positions as part of the skill execution. Cam and pincer lesions are the two varieties of FAI lesions, and these can combine to form double lesions. Conservative management usually fails in the young athlete to completely manage their pain. Therefore surgery, either open or arthroscopic, is usually the recommended treatment. Post-operative rehabilitation is addressed in part II of this series.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Further reading
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









