Plantar plate tear: a common overload injury in athletes

Pain under the metatarsal-phalangeal (MTP) joint is common in athletes and a tear or rupture to the plantar plate may be responsible for pain in this area. Plantar plate injury can occur under any of the metatarsals; however injury at the 2nd MTP joint is most common, as it is the longest metatarsal and has unopposed lumbricals and no plantar interosseous insertions. This condition is also known as pre-dislocation syndrome, crossover toe deformity, and floating toe syndrome(1).
Anatomy and biomechanics
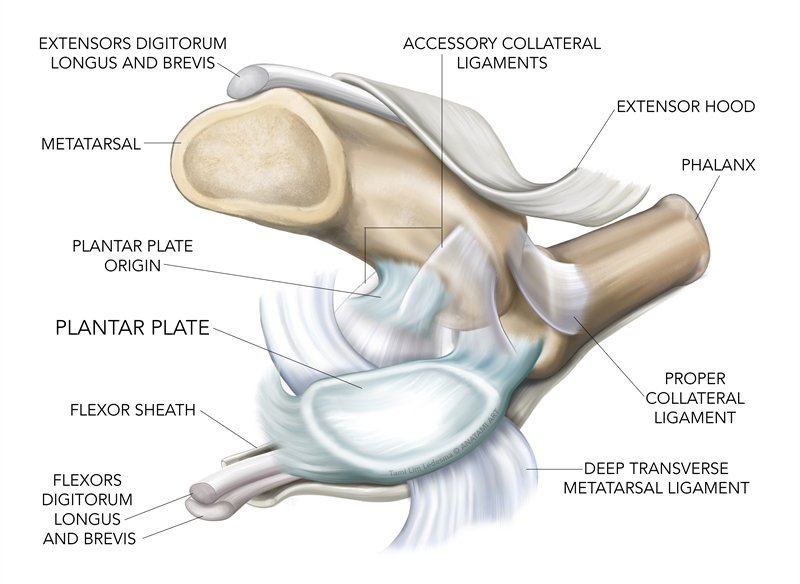
The plantar plate of the MTP joint is a broad, rectangular to trapezoid shaped ribbon-like disc that is a fibrocartilaginous thickening of the MTP. On average it is 16mm long, 9mm wide, and 1.8mm thick(2,3). The plate originates on the periosteum of the shaft of the metatarsal and inserts onto the proximal phalanx as a strong attachment. The mid-portion of the plate is the thickest - corresponding to an area where the MTP joint would dorsiflex - and at this point it also provides an attachment point for the collateral ligaments, deep transverse metatarsal ligaments, and fibers from the plantar aponeurosis(2). The flexor tendon sheaths adhere to the borders of the plantar plate and together they act as a flexor pulley system(4). In addition, the plantar plate of the 1st MTP joint has the sesamoid bones as part of the complex (see figure 1).Figure 1: Anatomy of the plantar plate
The plantar plate needs to be both stable and flexible. Flexibility allows dorsiflexion of the MTP joint, and also provide a firm, strong structure that can withstand tensile loads. Furthermore, the plantar surface allows for a smooth gliding motion of the flexor tendon complex(2). The primary functions of the plantar plate are to(2-4):
- Stabilize the MTP joint and resist hyperextension (dorsiflexion) of the joint.
- Assist in the windlass mechanism through the attachment to the plantar fascia,.
- Absorb compressive loads along with the fat pad of the metatarsal heads.
Injuries to the plantar plate
Tears of the plantar plate may occur in the 1st MTP joint and is termed ‘turf toe’. Acute plantar plate tears at the 1st MTP joint are relatively common in athletes who wear flexible shoes and compete on artificial surfaces(4). A sudden aggressive dorsiflexion movement of the MTP leads to a rupture of the plantar plate.Plantar plate injuries are actually more common at the 2nd MTP joint, which has the longest metatarsal, unopposed lumbricals, and no plantar interosseous insertions. These tears arise from the base of the proximal phalanx, and are caused by repetitive overload from abnormal forefoot loading. Hallux valgus, excessive pronation, a short first metatarsal, or a long second metatarsal can cause overloading in this area.
When ruptured, the proximal phalanx assumes a dorsally subluxed position due to the disruption of the passive stabilizing structures, combined with the pull of the flexor tendon pulley system under the MTP(4). This may cause the 2nd toe to migrate over the 1st toe and create a ‘crossover toe’ sign(6,7). Other pathologies can also cause pain under the MTP, mimicking a plantar plate tear or rupture(8). These include:
- Neuroma
- Fat pad atrophy
- Metatarsalgia
- Metatarsal head overload
- Capsulitis and synovitis
- Lesser metatarsal stress fractures
Diagnosis
An athlete who suffers a plantar plate tear may recount an acute dorsiflexion type mechanism of injury, or they may develop pain under the MTP over an extended period of time. Some of the features of a tear to the plantar plate can include:- Localized pain under the MTP joint.
- Swelling extending to the dorsal aspect of the joint.
- Symptoms imitating compression syndromes of the plantar digital nerves (due to fluid compression of the nerves).
- Pain exacerbated by passive and/or active dorsiflexion of the MTP.
- Pain that is usually consistent and constant, and does not vary much based on activity.
- An anterior-posterior draw test (Modified Lachman’s Test) demonstrating laxity of 2mm or greater than 50%.
- A 2nd toe that moves medially, with a greater spread between the 2nd and 3rd
- A positive plantar grip test. This is assessed by using an 8cm x 1cm strip of paper placed under the 2nd toe of the standing patient to evaluate if the patient is able to ‘grip’ the paper(9).
Imaging
An ultrasound scan may show hypoechoic defects in the plate, usually at the distal attachment. An arthrogram may show synovial hypertrophy and seepage of the dye into the flexor tendon sheath. Magnetic resonance imaging typically shows fluid in the plate and a loss of continuity in the tissue and are more sensitive in diagnosing plantar tears than an ultrasound (10). An MR arthrography is the gold standard imaging modality for this injury. This test detects dye extravasation from the MTP joint into the flexor tendon sheath, suggesting a rupture that creates an opening(11). X-ray radiographs are not normally the imaging modality of choice but they may show a superior migration of the proximal phalanx.Injury grading
Nery et. al. proposed a classification system that assigns the grade of injury depending on the pathophysiology of the injury, the relevant signs and symptoms, and the results of imaging studies (see table 1)(12).| Grade | Signs and symptoms | Anatomical features |
|---|---|---|
| 0 — MTP aligned, prodromic stage with pain with no deformity | · Joint pain in MTP· Thickening and swelling MTP· Weak plantar grip· Negative drawer test | · Attenuation and/or discoloration of the plantar plate |
| 1 — Mild MTP displacement, widening of space between toes, medial displacement | · Pain in MTP· Swelling in MTP· Diminished plantar grip· Less than 50% subluxation on drawer test | · Distal transverse lesion (adjacent to insertion).· Proximal phalanx (<50%)· May be medial, lateral, or central lesion |
| 2 — Moderate displacement and deformity (either lateral, dorsal or dorsomedial), hyperextension of big toe | · Joint pain· Minimal edema· No plantar grip· Less than 50% on drawer test | · Distal transverse lesion (>50%)· Medial/central/lateral area and/or intrasubstantial lesion |
| 3 — Severe displacement, dorsal or dorsomedial deformity, 2nd toe may overlap, flexible toe clawing may be present | · Pain in joints and feet· Not much swelling· No plantar grip· MTP dislocated on drawer test· Flexible toe clawing | · Transverse lesion and/or extensive longitudinal lesion (may involve collateral ligaments) |
| 4 — Dorsomedial or dorsal displacement, severe deformity with dislocation, fixed toe clawing | · Pain in joints and feet· Minimal swelling· No plantar grip· MTP dislocated on drawer test· Fixed toe clawing | · Extensive lesion in buttonhole shape· Combination of transverse and longitudinal plate injuries |
Injury management
Depending on the grade of injury, the plantar plate may be deemed stable or unstable. As with many orthopedic conditions, stable conditions may be treated conservatively while unstable injuries need surgical intervention to obtain a positive outcome (see table 2).*Conservative treatment
Patients should rest and use protective strapping with padding to unload the plantar plate. The patient may feel supported with orthotics and stiff sole shoes, or rocker-bottom boots. Often the patient will be placed in a CAM walker (moon boot) and be non-weight-bearing for the first two weeks with gradual progression to partial then full-weight-bearing over a six week period. Insert an insole foam pad with a space cut out for the affected MTP to unload the area. To further protect the MTP, tape it to prevent excessive dorsiflexion.| Phase one | |
| Aim | To decrease pain, reduce swelling and maintain range of motion at associated joints. |
| Timeline | 0-2 weeks. |
| Interventions | Ice for pain, protective strapping, talocrurual, and midfoot mobilizations, gentle towel scrunchies. |
| Phase two | |
| Aim | Increase weight bearing, normalize gait, improve ROM, strengthen foot and calf muscles. |
| Timeline | 2-6 weeks. |
| Interventions | Gradual weight bearing, customized orthotic, towel exercises, maintain talocrural and midfoot mobilizations, gentle grade 1-2 MTP moves, stability exercises for the toe. |
| Phase three | |
| Aim | Increase strength, improve proprioception. |
| Timeline | 6-10 weeks. |
| Interventions | Calf raises, high-level intrinsic muscle activation, return to sport. |
*Surgical treatment
Patients that fail conservative management may need surgical correction of the plantar plate with or without a flexor tendon transfer. It is beyond the scope of this article to outline the various surgical options available to correct the plantar plate tear; however, it may require a direct repair of the plantar plate, a tendon transfer operation, or both. If the underlying anatomy is a factor in producing the tear, the patient may require a 2nd metatarsal osteotomy. Interested readers are directed to the review by Baravarian et al (2011)(8) for the criteria used to determine the type of corrective surgery needed.Summary
A tear/rupture of the plantar plate of the MTP joint can cause pain and dysfunction in the MTP of an athlete. Although they may occur at any MTP, the 2nd MTP is the most commonly injured. This is often caused by an overload to the MTP joint due to repetitive compression, shear, and tensile forces. Those with anatomical variants to the metatarsals have an increased risk of this type of injury. Conservative management of a stable plantar plate injury may take up to 10 weeks, and unstable injuries with deformity may need surgery with protracted rehabilitation periods.References
- Brukner and Khan (2017) Clinical Sports Medicine. McGraw Hill. Australia
- Foot and Ankle International. 1995; 16(8). 480-486
- Magn Res Imaging Clinics N Am. 2001; 9(3); 659-69
- Surg Radiol Anatomy. 2007, 29(2); 141-147
- Am J Sports Medicine. 1990. 18; 280-285
- Foot Ankle. 2000; 21(5). 375-378
- Foot Ankle. 1997. 8(1): 29-39
- Clinical Podiatry Med Surg. 2011; 28; 57-68
- J Foot and Ankle Surgery. 2013; S1067-2516(13); 00106-3
- J of Orthopaedic Surgery and Research. 2017; 12. 14
- J Foot and Ankle Surgery. 2004; 43(4): 266-270
- Rev Bras Orthop. 2015; 50(6); 720-728
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










