Relative energy deficiency in sport (RED-S): What all health professionals need to know
Dr Nicola Keay explains the phenomenon of energy deficiency in sport, the impacts on athlete health, and also provides advice for professionals with athletes in their care.

2016 Rio Olympics - Badminton. Sung Ji-Hyun (KOR) of South Korea has something to eat during a break. REUTERS/Marcelo del Pozo
The female athlete triad model describes a clinical spectrum of nutrition, menstrual function, and bone health. The spectrum ranges from appropriate nutritional practices, regular menstrual function, and good bone health through to eating disorders, amenorrhoea (lack of periods), and osteoporosis.
Exercising females report a high incidence of menstrual dysfunction. That is not to say that menstrual dysfunction is an inevitable, or acceptable outcome of exercise in women. Regular menstruation demonstrates healthy hormone levels. Therefore, irregular menstrual cycles indicate hormone irregularities. Hormones, both short and long-range/term are key to driving the beneficial adaptations to exercise. Females who lack normal hormone activity likely sacrifice performance as well as adaptations.
What is RED-S?
The limitation of the female athlete triad is that this model excludes half the population. The RED-S clinical model first described by the International Olympic Committee (IOC) in 2014 incorporates the female athlete triad and, importantly, also includes males. Furthermore, the RED-S model describes multisystem effects, which are not limited to menstrual function and bone health.
In both the female athlete triad and RED-S, the underlying issue is that of low energy availability (LEA). Typically the value of energy availability (EA) required to maintain resting metabolic rate is quoted as 45Kcal/kg of FFM (fat-free mass), which takes into account that there will be variations between individuals depending on their body composition. However, be aware that this value of EA is not an absolute threshold applicable to everyone. Instead, it is a guide. An athlete can end up in LEA either unintentionally or intentionally.
Calculating Low Energy Availability
For a detailed explanation of how to calculate low energy availability and its role in recovery, see Alicia Filley’s article on RED-S.
In the central column of figure 1, the athlete/dancer has adequate EA, as energy intake is sufficient to cover both energy demands from training and to maintain health. However in the column to the left, restriction of intake, whilst maintaining same training load results in LEA. In right column, although energy intake has been maintained, there is a higher energy demand from increased training load, resulting in LEA.
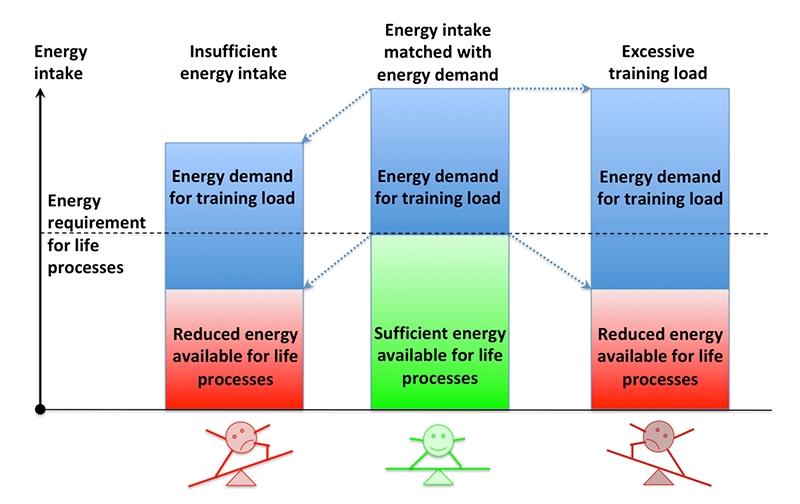
Figure 1: Scenarios of low energy availability*
*Dr N Keay BJSM 2018
EA is a very useful concept for athletes/dancers. They can optimise EA through integrated periodisation of the three key variables under their control: training load, nutrition and recovery. Achieving optimal balance and timing of these factors will mean adequate EA to support health and therefore athletic performance shown in figure 2 by the green central area of the equilateral triangle. Conversely non-integrated periodisation of these inputs results in suboptimal health and performance falling off into red peripheries.
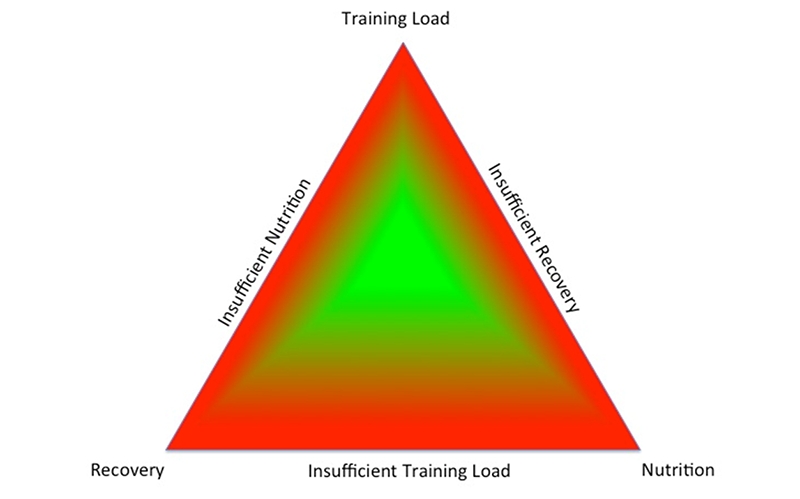
Figure 2: Integrated periodisation supports optimal health and performance*
*Dr N Keay BJSM
Who is at risk of RED-S?
Any exerciser, of any age or level can be at risk of developing LEA and therefore the health and performance consequences of RED-S. There is an increased risk in certain gravitational sports (where power-to-weight ratio is important) such as running, cycling and climbing(1). Weight category sports like boxing, martial arts, light weight rowing also carry increased risk as do aesthetic sports, such as gymnastics and diving(1). Although not a sport, dancers are at high risk of developing LEA and RED-S. This is because being lightweight not only confers a performance advantage but is also encouraged as an aesthetic requirement.
Male cyclists are at risk of poor bone health on two fronts. Road cycling as a non-impact exercise, does not provide osteogenic stimulus. In addition, a low bodyweight confers a performance advantage by providing a higher power-to-weight ratio (watts per kilo) which helps overcome gravity and propel the rider up inclines.
Unlike weight-bearing sports, where a stress fracture would be an early warning sign of poor bone health due to LEA, the first sign of low bone mineral density (BMD) in a cyclist is usually a serious fracture. Vertebral fractures may require surgery, and substantial time away from training. In cyclists, the lumbar spine is most often affected by RED-S. The type of bone in the these vertebra are particularly sensitive to hormones and nutrition. As you can see in figure 3, the 50 male cyclists in our recent study demonstrated low BMD at the lumbar spine (the ‘Z score’ is an age-matched measure of BMD - anything negative is below normal). Those riders with LEA showed dramatically low BMD.
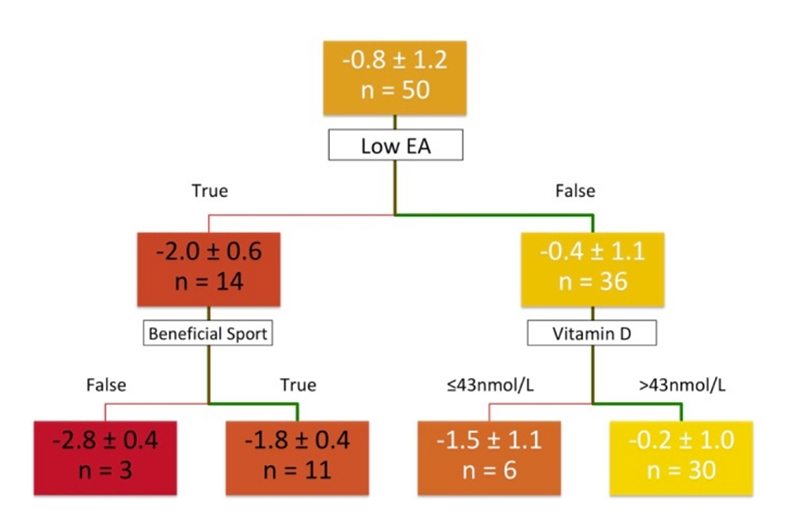
Figure 3: Male cyclists and bone mineral density (BMD) of the lumbar spine*
Male cyclists with low energy availability showed a poor Z score (-2.0) compared to cyclists who didn’t have LEA (Z score of -0.4). Furthermore, cyclists with LEA and who didn’t participate in another beneficial sport (such as running or weight training, which stimulates BMD) showed an even worse Z score of -2.8)
*Source: Dr N Keay, BMJ Open Sport Exerc Med. 2018; 4(1): e000424.
Young athletes are particularly vulnerable to RED-S. In the first instance, they are at high risk of developing LEA - being already in a high energy demand due to their state of growth and development. Secondly the adverse consequences of LEA are likely to have longer-term effects. For example, attenuation of the accumulation of peak bone mass (PBM) during adolescence increases the risk of developing stress fractures when training loads increase moving from junior to senior ranks, or from dance training to professional dance company.
So what?
Healthy hormones drive beneficial adaptations to exercise training and support full performance potential. Training only produces positive effects with adequate EA and therefore a fully functioning endocrine system, rather than one on energy-saving mode. An example of this is shown graphically in figure 4; male cyclists in chronic LEA did not achieve the expected performance from their increased training load when compared to controls consuming adequate energy,
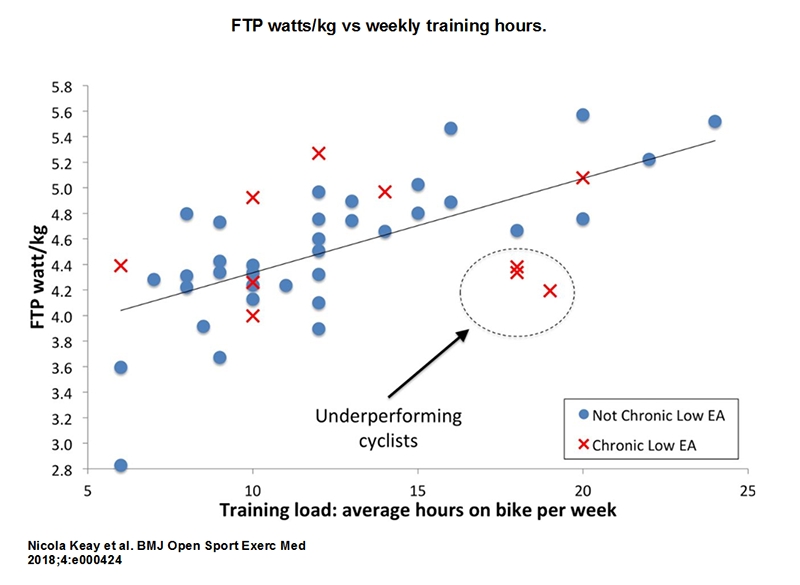
Figure 4: Training load, EA and fitness gains
The overall trend reveals that when EA is adequate, increasing training load is associated with greater functional threshold power (watts/kg). However, when there is chronic low EA, increasing training loading is associated with underperformance.
Identifying those at risk of RED-S
In surveys of female athletes, the majority were not fully aware of the implication of menstrual disruption on bone health (95% in US study and 45% in Australia)(2). For male athletes there is even less information. Fifty percent of healthcare professionals are not fully aware, or know how to identify those at risk of RED-S according to the IOC update on RED-S 2018. [For more on incorporating RED-S screening into an injury evaluation, see Alicia Filley’s article]
Although LEA is the fundamental issue in RED-S, there are major issues with quantifying EA. In the first instance, quantification of EA in ‘free living’ athletes is inaccurate and laborious. Even if a value is calculated, there is no absolute threshold below which all athletes will develop a set degree of endocrine dysfunction. The calculated value for EA is only applicable at the time of measurement.
Endocrine markers have been shown to be more objective and quantifiable indicators of an individual’s functional response to EA without a temporal dimension(3). Furthermore, this functional response to EA has been linked to clinical outcome of stress fracture, known to be a performance limiting effect of RED-S(4). However the story doesn’t end there. A validated questionnaire for female athletes called LEAF-Q has been developed to detect those at risk of LEA. But what about male athletes?
Until our recent study of male cyclists (BMJ Open Sport Exerc Med. 2018; 4(1): e000424), there was no equivalent. From this study, a specially designed Sport Specific Energy Availability Questionnaire and Interview (SEAQ-I) was found to be the variable most indicative of the ‘gold-standard’ indicator of RED-S - namely the Z score of the lumbar spine as shown above in figure 4. This is an important development. Potentially athletes and coaches could use such screening tools to identify those at risk of LEA before the adverse effects of RED-S occur.
How to manage those identified with RED-S?
Once an athlete is identified as being at risk of RED-S, what should be done? In the first instance this situation needs discussing with athlete, coach, parent (if a young athlete). Be aware that RED-S is a diagnosis of exclusion. In other words early medical input is important to rule out any underlying medical issues such as infection, inflammation or an endocrine condition per se. Once this has been done, there are clinical assessment tools to classify the athlete according to symptoms and signs of LEA. This comprises of three categories: green (good to go), yellow (proceed with caution, reduce training load and increase energy intake) and red (stop due to a serious risk to health).
Note that pharmacological intervention in terms of oestrogen and cyclic progesterone for female athlete is only appropriate in cases of arrested puberty with primary amenorrhoea and secondary amenorrhoea, where there is evidence of serious bone health issues. In all cases this treatment should only be used in conjunction with a strategy to address EA issues - NOT as a replacement for this. In the case of male athletes, there is no justification for therapeutic use exemption (TUE) for testosterone; in RED-S, a low testosterone level is a result of non-integrated periodisation of training and nutrition, therefore not a medical condition per se.
Recommendations
LEA is the underlying issue of the adverse health and performance consequences of RED-S, and EA is under the control of the athlete. Supporting these athletes should be based on empowering them to take control and review the truimverate of training load, nutrition and recovery, with guidance from healthcare professionals, clinical dieticians, coaches and parents/friends. This is the objective of the free and open access educational website Health4Performance (health4performance.co.uk/healthcare-professionals/), for which you can find the link below.
Useful references and information for further reading
- Expanding the female athlete triad: relative energy deficiency in sport affects men too
- Health4PerformanceBASEM open access educational website
- Low energy availability assessed by a sport-specific questionnaire and clinical interview indicative of bone health, endocrine profile and cycling performance in competitive male cyclistsDr N Keay, G Francis, K Hind, BMJ Open
- 2018 UPDATE: Relative Energy Deficiency in Sport (RED-S)Dr N Keay, BJSM
- Raising Awareness of RED-S in Male and Female Athletes and DancersDr N Keay, BJSM
- What is Dance Medicine?Dr N Keay, BJSM
- Optimal Health: Especially Young Athletes! Part 3 - Consequences of Relative Energy Deficiency in SportsDr N Keay, BASEM
- How do you identify male cyclist at risk of RED-S?Dr N Keay, BJSM
- Cyclists: Make No Bones About ItDr N Keay, BJSM
- Male Cyclists: bones, body composition, nutrition, performanceDr N Keay, BJSM
References:
- Cur Rev in Musc Med. June 2013;Volume 6 (2):195–204
- blogs.bmj.com/bjsm/2018/02/18/cumulative-endocrine-dysfunction-relative-energy-deficiency-sport-red-s/
- International Journal of Sport Nutrition and Exercise Metabolism 2018; 28(4): 403-411
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









