Fractures of the Proximal 5th Metatarsal in Athletes

First described in 1903 by Sir Robert Jones(1), fractures of the fifth metatarsal (MET) are relatively common fractures of the foot(2). The estimated incidence of fifth MET fracture is 1.8 per 1000 person-years(3,4), and 68% of MET fractures are fractures of the fifth MET, the majority of which are proximal(5). Furthermore, fractures most commonly occur in the 20-60-year-old age group(6) and more frequently in younger males and older females(7,8). A more detailed analysis of fracture risk suggests the following factor increase risk:
- Longer 5th MET(9)
- Higher medial longitudinal arch(9)
- Increased 5th MET adduction angle(10)
- Shoe design(11)
- Vitamin D deficiency(12)
- Non-dominant foot in footballers(11)
- Harder play surfaces(13)
- Increased loading(13)
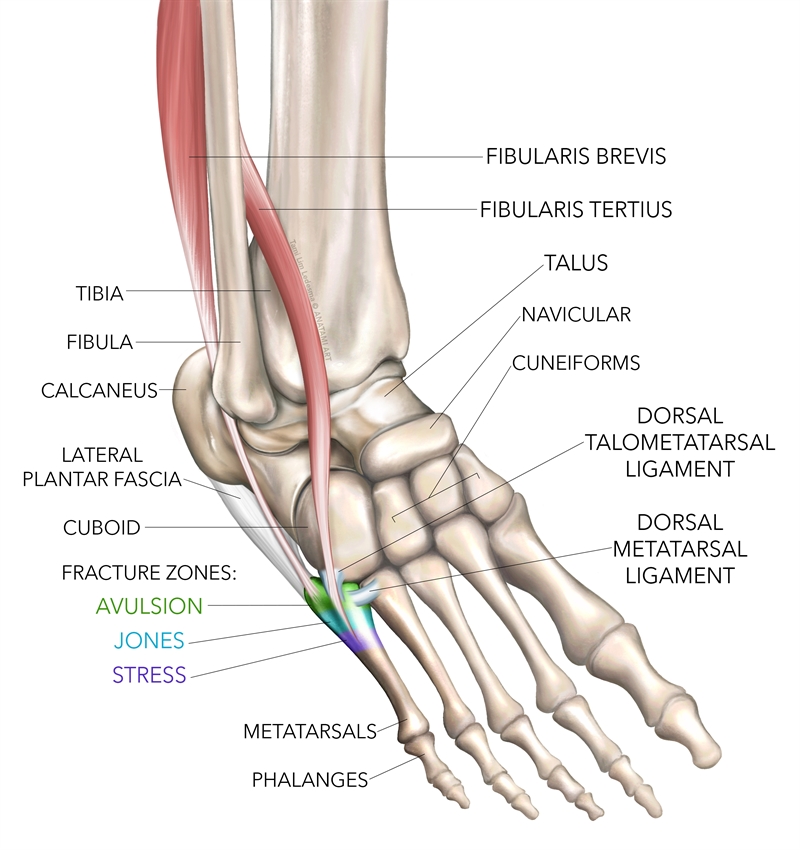
Anatomy and biomechanics
The proximal base of the fifth MET is firmly attached to the fourth MET and cuboid bone via strong ligaments (see figure 1). These ligaments terminate at the junction between the metaphysis and diaphysis. The sturdy ligamentous attachment to these midfoot bones directs stress from the mobile head of the MET to the more rigid base. The metaphysis-diaphysis junction, therefore, acts as a fulcrum between the head and base of the MET(7,14,15). This relevant anatomical and biomechanical feature means that strong vertical or medial/lateral forces applied to the fifth MET may cause a fracture distal to the rigid base(16).The first and second MET absorb the most peak forces during running, followed by the fifth MET. However, the relatively low cross-sectional area (thinness) of the fifth MET cortex makes it relatively weaker, and therefore more prone to fracture(17). Finally, the lateral aspect of the fifth MET endures the greatest tensile and torsional force when running. When fractured, this may cause the healing ends to gape and lead to higher rates of non-union(18,19).
Other anatomical factors may play a role in fractures of the base of the MET. The lateral band of the plantar fascia attaches to the plantar aspect of the tuberosity on the distal end of the fifth MET; the peroneus brevis attaches to the dorsolateral aspect, and; the peroneus tertius attaches to the dorsal metaphysis(20-22). These attachments relate to avulsion fractures of the tuberosity or Zone-1 fractures.
Figure 1: Anatomy of the fifth metatarsal
The sparse circulation to the fifth MET, supplied by a network of three arterioles, is another relevant anatomical factor. This network consists of(23):
- The periosteal arteries.
- The nutrient artery, which enters the middle third of the diaphysis and branches proximally and distally.
- The metaphyseal perforators located around the metaphysis. A ‘watershed’ zone exists between the nutrient artery and the metaphyseal perforators. Due to the poor blood supply in this area, there exists a higher chance of delayed union and non-union of fifth MET fractures(22,24).
Fracture classification
The seminal paper by Sir Robert Jones in 1903(1), initially led medical practitioners to term all fractures of the proximal fifth MET as Jones Fractures. In the ensuing decades, however, classification systems have become more detailed concerning the anatomical location of proximal fifth MET fractures. Lawrence and Botte described the most commonly used classification in 1993(25). This system distinguishes three types of proximal fifth metatarsal fractures based on the mechanism of injury, location, treatment options, and prognosis.- Zone 1 fractures (avulsion fractures of the tuberosity) - By far, the most common, accounting for 93% of all fifth MET fractures, these are caused by inversion injuries, which cause the peroneus brevis to traction its tendon attachment away from the bone. These usually begin laterally on the tuberosity and extend proximally into the metatarsocuboid joint, spreading across an area of cancellous bone with a good blood supply. As a result, Zone-1 fractures are common. Usually they have good outcomes with conservative treatment, such as early weight-bearing using an orthopedic shoe or moon boot, or a Jones bandage dressing – a bulky compression dressing used to immobilize the area(26-28). However, if the fracture is displaced more than 2-3mm, is comminuted(7), involves more than 30% of the cuboid-metatarsal articulation, or has large avulsed fragments (with or without rotatory components)(29), it is usually a candidate for surgical fixation(30). Fractures with more than a 2mm step off involving the joint surface require open reduction fixation(31).
- Zone 2 fractures (metaphyseal-diaphyseal - the classic ‘Jones’ fracture) – This transverse fracture at the metaphyseal-diaphyseal junction does not extend further than the fourth and fifth metatarsal articulation. An adduction force to the plantarflexed forefoot (a stepping and cutting type movement), creates a bending moment on the plantar aspect of the fifth MET starting at the proximal fulcrum and causes a Zone-2 fracture(32). Treat this area of inadequate blood supply surgically to avoid delayed union, non-union, or refracture(33,34).
- Zone 3 (diaphyseal) fractures - distal to the tuberosity (proximal 1.5cm of the diaphysis) – These are stress fractures, which in athletes are more prone to delayed union or even non-union. Zone-3 fractures require more specialized treatment strategies. These fractures are typically due to overload on the midfoot and forefoot from running and cutting movements. They are the most common type of metatarsal stress fracture, especially in young athletes in early pre-season training, where there are high running loads(35). Interestingly, the most pressure difference between the base and head of the fifth MET occurs during acceleration, and some authors suggest monitoring acceleration loads in training as a preventative measure(36).
Subtype categories for Zone 2 and 3 fractures help practitioners decide on the most suitable treatment plan(33):
- Type I (acute) - A narrow fracture with no intramedullary sclerosis.
- Type II (delayed union) - A wide fracture line and intramedullary sclerosis.
- Type III (non-union) - A fracture with complete destruction of the medullary canal by the sclerotic bone.
The typical treatment options are summarized below;
- Zone-2, type-1 fractures – Non-weight bearing, short leg cast for 3-12 weeks(33).
- Zone-2, type-2 fractures - May be treated conservatively as above. However, early surgical treatment reduces the time of the union and the time of immobilization.
- Zone-2, type-3 fractures - Managed surgically.
- Zone-3 fractures - Representing the accumulative ‘stress’ type fractures (whereas Zone-2 Jones fractures are often traumatic)with prolonged healing times and a high chance of non-union(7). Conservative treatment in a non-weight bearing short leg cast for at least 6-8 weeks for non-athletic populations is the first line of treatment. However, athletes will often need surgical intervention(37,38).
Diagnosis
Athletes who present with a fracture to the proximal fifth MET may describe the following signs and symptoms(39):- An episode of acute trauma or repetitive trauma to the foot.
- An event with strong plantarflexion/inversion as an injury mechanism (in Zone-1 fractures).
- A large adduction force applied to a foot that is in plantarflexion (in Zone-2 fractures).
- Pain with walking and running.
- Pain on direct palpation of the fifth MET.
(NB Zone-3 fractures are stress-related, and often, athletes may not remember an acute precipitating event.)
If a fifth MET fracture is suspected, plain films will show occult and obvious fractures in Zone-1 and 2 type fractures. Zone-3 (stress) fractures will most likely need more detailed imaging such as CT scan, bone scan, or MRI(4) (see figure 2).
Figure 2: MRI showing a Zone-3 fracture of the 5th MET (stress fracture)*

*Image reproduced with permission from Stress Fractures in the Foot and Ankle, William N. Snearly, M.D.
Surgical options
Because of the relatively high non-union, delayed union, and refracture rates in athletes, researchers continue to seek the best surgical fixation devices for fifth MET fractures. Surgeons describe a few variations in surgical techniques, such as intramedullary screws, tension band wiring, differential pitch screw, and percutaneous bi-cortical screw fixation⁴¹. Intramedullary compression screw (4.5 mm) with or without bone grafting appears the most common choice for surgeons(30,34,42) and has a high success rate(43). However, some report complications of screw fixation in athletes, including delayed and non-union(44), and similarly with tension band wiring(14). Plate fixation on the plantar aspect and lateral side of the fifth metatarsal shows good results since it provides better resistance to rotational and tensile forces(45).Post-op rehab
The postoperative period usually begins with immobilization in a short leg cast or plaster splint for one to two weeks, followed by a walking boot(46,47). Patients may start progressive weight-bearing from week four onwards. By six to eight weeks post-operatively, athletes can walk with full weight-bearing and resume normal activities. In cases of post-surgical Zone-3 stress fractures of the proximal diaphysis, some authors suggest an extension of the initial period of cast immobilization and non-weight bearing to six weeks(14).Athletes can return to sports training when there is radiological evidence of union and a resolution of symptoms(44). The time between the radiological union and pain-free sports participation is quite varied; studies indicate a return to sport may be possible as soon as three weeks post-surgery, while others suggest return-to-sport after four to five months(48).
References
- Ann Surg. 1902;35(6):697–700 2
- The Foot. 2001;11(2):99–102
- Orthopaedics 2001;24:204–8
- J Bone Joint Surg Am 2003;85-A:820–4
- Foot Ankle Int. 2006;27(3):172–4
- Acta Orthop Scand. 1994;65(5):545–7
- J Am Acad Orthop Surg. 1995;3(2):110–4
- The Foot. 2004;14(2):96–8
- The American Journal of Sports Medicine 2020;48(2):424–431
- J Foot Ankle Surg. 2012;51(6):739-742
- Clin J Sport Med 2014. 24(1):58–61
- Foot (Edinb). 2016 Jun;27:50-2
- Knee Surgery, Sports Traumatology, Arthroscopy. 2019; 27:2796–2801
- Knee Surg Sports Traumatol Arthrosc. 2011;19(5):853–7
- The Foot. 1998;8(1):38–45
- J Bone Joint Surg Am 1978;60:776–82
- Am J Sports Med 1989;17:669–74
- Am J Sports Med. 2011;39(10):2206-2211
- Foot Ankle Int. 2004;25(9):650-656
- J Foot Ankle Surg. 2015;54(1):94–8
- J Trauma 1980;20(6):530–1
- Am J Roentgenol 1984;143:889–91
- Foot Ankle. 1992;13(3):143–52
- Foot Ankle 1991; 11:350–353
- Foot Ankle. 1993;14(6):358–65
- Foot Ankle Surg. 2011;17(4):300–7
- Int Orthop. 2007;31(1):5–10
- Foot Ankle Int. 2007;28(5):581–3
- Am J Sports Med 1992; 20:50–54
- 2010;41(6):555–62
- Skeletal Radiol 2014; 43: 467-474
- Orthop Clin North Am 1995; 26(2):353–61
- J Bone Joint Surg Am. 1984;66(2):209–14
- Am J Sports Med. 2005;33(5):726–33
- Scand J Med Sci Sports 2012;22(3):341–6
- Phys Sportsmed 2009;37(2):87–92
- Orthop Clin North Am. 2001;32:171–180
- J Am Acad Orthop Surg. 2000;8(5):332–8
- World J Orthop 2016 December 18; 7(12): 793-800
- Am J Sports Med 2007;35(4):643–9
- Arch Trauma Res. 2016 December; 5(4):e33298
- Acta Ortop Bras. 2012;20(5):262–5
- Foot & Ankle International. 2020. 1– 8 DOI: 10.1177/1071100719898278
- Am J Sports Med. 2002;30(1):55–60
- Foot and Ankle International 2020. 1-9. DOI: 10.1177/1071100719895273
- Am J Sports Med. 1983;11(5):349–53
- Clin Orthop Surg. 2011;3(2):140–6
- Knee Surg Sports Traumatol Arthrosc. 2013; 21:1307–1315
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.