Hip avulsion injuries: getting the full management picture

As discussed in part one of this article, the presentation and location of a hip avulsion injury can vary greatly. This is due to the complex musculotendinous anatomy in the region, and the various precipitating movements causing either an acute tear or a chronic strain. Therefore, imaging studies are an essential component of an accurate diagnosis, which then determines the optimum treatment or management plan.
Imaging for hip avulsion injury
Choosing the appropriate imaging test can provide confirmation of a suspected hip avulsion injury. Plain X-ray imaging is usually sufficient to make a diagnosis, if it is supplemented by oblique or axial projections of the affected area(1,2). However, research on athletes suggests that in order to distinguish a true avulsion fracture from the unfused apophysis, images of the affected side should be compared with the unaffected side(3).In most avulsion fractures, conventional radiography typically shows a displaced fracture fragment at the origin or insertion of a muscle or tendon (see figure 1). Further testing with CT, MRI, or ultrasound imaging is not usually required(4). The caveat, however, is in adolescent athletes or children; plain radiographs can be interpreted as negative when an apophyseal avulsion is non-displaced or when the apophysis is unossified(5). In such cases, the use of ultrasound or MRI can prove helpful(6).
Figure 1: X-ray imaging showing displaced fracture fragment
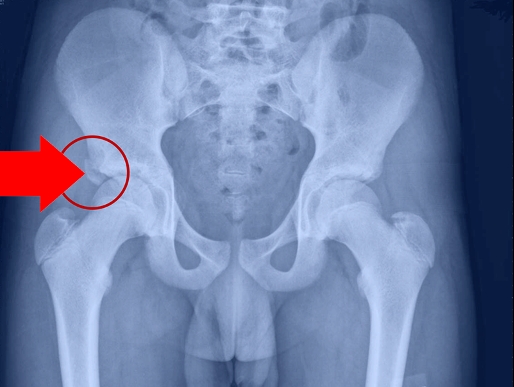
An anteroposterior pelvic radiograph showing the avulsed fragment of the lateral aspect of the right acetabulum (identified by arrow).
Researchers in Germany demonstrated the benefits of using ultrasound imaging in the case of apophyseal avulsion fractures in the less mature skeleton(7). They examined 243 young athletes, using both radiography and ultrasound, where there were clinical suspicions of apophyseal avulsion fractures. In 80 cases, the diagnosis was confirmed by radiographs, whereas ultrasound imaging confirmed the diagnosis in 97 cases.
MRI and CT imaging can also play a useful role in imaging as part of a diagnosis. In fractures where there is minimal displacement of the avulsed ossified apophysis, plain radiography may be negative despite a high degree of clinical suspicion. Consider the use of CT imaging in these circumstances as a follow up due to its enhanced sensitivity(4). MRI imaging is able to reveal hematoma and periosteal stripping at the tendinous attachment sites, as well as ‘waviness’ and retraction of the torn end of the tendon(3). The degree of tendon retraction influences the prognosis of the lesion, particularly in hamstring lesions, which are prone to significant tendon retraction. Indeed, if the hamstring tendon is retracted by more than 2cms, this may result in abnormal healing and extended disability for the athlete(4).
Chronic avulsion injury and imaging
In cases of chronic avulsion injury where there is no acute event precipitating an injury, plain radiography may be less informative. For example, in distal chronic avulsive adductor insertion syndrome (more commonly known as thigh splints), plain radiography is rarely diagnostic in the early phase, although it can reveal limited periosteal bone apposition at the medial proximal third of the femur in advanced cases(8).When clinicians suspect a chronic avulsion injury, radiography alone may not be sufficient to make a diagnosis. Instead, MRI and scintigraphy (where small amounts of radio tracers such as technetium 99 are used to create gamma-ray imaging of skeletal tissue – also known as a gamma scan) are recommended. Scintigraphy exploits the fact that chronically stressed or injured skeletal tissue undergoes greater metabolic turnover than neighboring regions; since more radio tracer is taken up by compromised skeletal tissue, this tissue is revealed as a ‘hot spot’ even though no morphological changes are apparent.
An MRI is useful for chronic avulsion diagnosis in the subacute and chronic stages since it can reveal soft tissue edema, as well as fatty replacement and sclerosis(3,9). In addition, it can also precisely identify the specific musculotendinous unit involved. Finally, it’s worth adding that MRI can also be useful in the healing phase to distinguish true non-union of an avulsed fragment versus a fibro-osseous union. Where there is non-union, MRI imaging shows a persistent high-intensity signal on T2-weighted images between the displaced apophyseal fragment and the underlying bone.
Avulsion treatment and management protocols
Because of the complex anatomy of the hip region, the wide range of possible injury locations and the differing precipitating injury mechanisms, it is not possible to make blanket recommendations on the most appropriate treatment and management protocols. In a large systemic review on avulsion injuries, researchers pooled data from 48 papers, the conclusions of which can be summarized as follows(10):- Treatment for avulsion fractures may consist of surgical or conservative interventions.
- The key determinant for the most appropriate treatment method will depend on the site of avulsion and the amount of displacement of the avulsed segment.
- Consider surgery in injuries where fragments are displaced more than 2cms
- Although many avulsion fractures can be treated conservatively, as many as 68% of avulsion injuries to the ischial tuberosity do not reunite, suggesting surgery may be more appropriate for injuries to this area.
- Compared to the general population, the argument for surgical intervention may be stronger for athletes who desire a speedy return to full function. However, some evidence suggests no significant difference between recovery times for surgical versus conservative interventions.
- Conservative treatment typically includes a period of bed rest for three days followed by a progressive program of ambulation. The progression involves a period of crutch use until the patient is able to walk without pain, followed by a continual increase of pain free activity. Return to full sport normally occurs six weeks post injury.
Location-specific recommendations
As mentioned above, the decision whether to treat conservatively or surgically is strongly influenced by the location and severity of the avulsion injury. Some of the key recommendations by location are as follows(11):- Iliac crest - This type of avulsion injury has an excellent outcome with conservative management. However, consider surgical management for a rapid rehabilitation with a quick return to sport or if the avulsed fragment is displaced more than 30mm.
- Anterior superior iliac spine - In the case of minimally displaced fractures, conservative treatment usually results in rapid healing of this injury. However, consider surgical management with open reduction and screw fixation in avulsions displaced by more than 15–20mm.
- Ischial tuberosity – Although surgery is more likely required, there is no consensus on the best treatment options for avulsion injuries of the ischial tuberosity and many centers still favor conservative treatment. However, consider open reduction and internal fixation if the avulsed fragment is displaced by more than 15mm.
- Pubic ramus and symphysis pubis – Manage these injuries conservatively with the cessation of sports activity and decreased weight bearing for a few weeks. Gradually increase loading as tolerated until a return to sport is possible.
- Greater trochanter – A rare injury, there is little available data regarding the best treatment of such avulsions. However, a conservative approach with restricted range of motion and cessation of sports for six weeks is recommended, especially in adolescents. Gradually increase loading as tolerated.
- Lesser trochanter – Most patients will respond well to conservative therapy and operative management is seldom required. A note of caution however: when a lesser trochanter avulsion is seen in mature adults, it can signify a pathologic avulsion fracture caused by metastatic involvement and requires further investigation(12).
Summary
Due to the complex etiology of hip and pelvic avulsion fractures, clinicians rely on comprehensive imaging to make an accurate diagnosis. Plain radiography is the starting point, but they may need additional imaging in the form of ultrasound, CT, MRI and scintigraphy. The best treatment option depends on the location of the injury and the displacement of the avulsed fragment. In many instances, a conservative approach involving limited weight bearing followed by a graduated loading program works well. However, surgical intervention may be recommended in more severe avulsion injuries, or where rapid return to play is a priority.References
- Skeletal Radiol 2001;30:127–31
- Skeletal Radiol 1996;25:3–11
- Radiol Clin N Am 2002;40:267–87
- Br J Sports Med 2007;41:827–831
- Eur J Radiol 2007; doi:10.1016/j.ejrad.2007.01.012
- Radiol Clin N Am 2002;40:333–62
- Knee Surg Sports Traumatol Arthrosc 1996;3:234–37
- Skeletal Radiol 1999;28:138–44.29
- Med Sci Sports Exerc 1990;22:436–43
- J Can Chiropr Assoc 2011; 55(4)
- Fortschr Röntgenstr 2020;192: 431–440
- J Orthop Case Rep 2017; 7: 16–19
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









