Acute Hamstring Injury Rehab – Get eccentric!
Patrick Gillham explores the benefits of using eccentric strengthening in rehabilitation for a quicker return to play following acute hamstring injuries.

West Ham’s James Collins holds his hamstring, 2016. Action Images via Reuters / Andrew Boyers
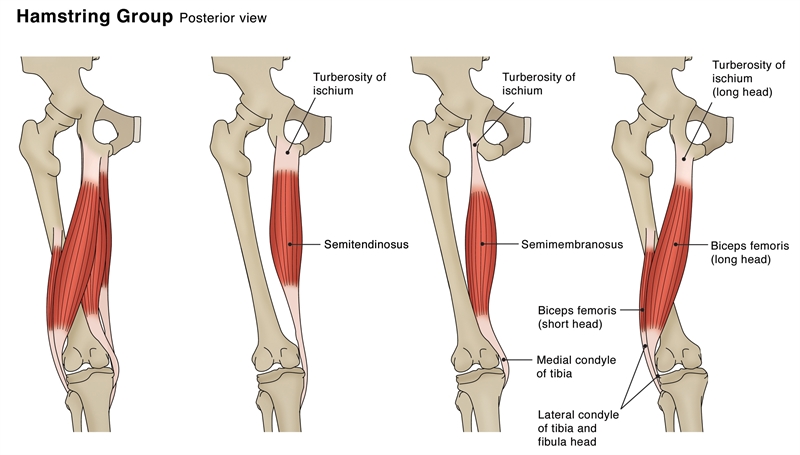
Figure 1: Hamstring Anatomy
Sporting activities involving high demands of sprinting or excessive stretching (kicking, sliding, split positions) have been found to influence the incidence of acute hamstring injuries. Hamstring injuries are diverse in nature, consisting of differing injury types, locations, and sizes. This makes recommendations regarding rehabilitation and prognosis about healing time and return-to-play notoriously difficult. It has been suggested that return to- play timescales vary between 28-51 days following acute hamstring injuries depending on the biomechanical cause, site, and grading of soft tissue injury(1). However, this is a contentious issue, which this article will explore.
Following a return to sport, the risk of re-injury is high within the first two weeks(2). The causes have been linked with initial hamstring weakness; fatigue; a lack of flexibility, and a strength imbalance between the hamstrings (eccentric) and the quadriceps (concentric)(2). The highest contributory factor, however, is believed to be an inadequate rehabilitation program, which coincides with a premature return to sport(3). More evidence is now highlighting the benefit of primarily using eccentric strengthening exercises in hamstring rehabilitation performed at high loads at longer musculotendon lengths(1,4).
Semitendinosus (ST), Semimembranosus (SM), and Biceps femoris long and short heads (BFLH and BFSH) make up the hamstring muscle group (see figure 1). They are involved with the extension of the hip, flexion of the knee as well as providing multi-directional stability of the tibia and pelvis. All three muscles cross the posterior aspect of both the hip and the knee joints, making them biarticular. As a result, they have to continuously respond to large mechanical forces created by upper limb, trunk, and lower limb locomotion via concentric and eccentric contractions. These forces are greatly increased during sporting activity, which is a likely culprit for their high injury frequency.
In a study at the University of Melbourne, biomechanical analysts quantified the biomechanical load (i.e., musculotendon strain, velocity, force, power, and work) experienced by the hamstrings across a full stride cycle during over-ground sprinting and compared the biomechanical load across each individual hamstring muscle(4).
Firstly, the hamstrings undergo a stretch-shortening cycle during sprinting, with the lengthening phase occurring during the terminal swing and the shortening phase commencing just before foot strike, and continuing throughout the stance (see figure 2). Secondly, the biomechanical load on the biarticular hamstring muscles was found to be greatest during the terminal swing.
BFLH had the largest peak musculotendon strain, ST displayed the greatest musculotendon lengthening velocity, and SM produced the highest musculotendon force as well as absorbing and generating the most musculotendon power. This ties in with other similar research, which distinguishes peak musculotendon strain as a large contributor to eccentric muscle damage, i.e., hamstring injury, rather than peak muscle force; hence the recommendation of eccentric strengthening for acute hamstring rehabilitation(1).
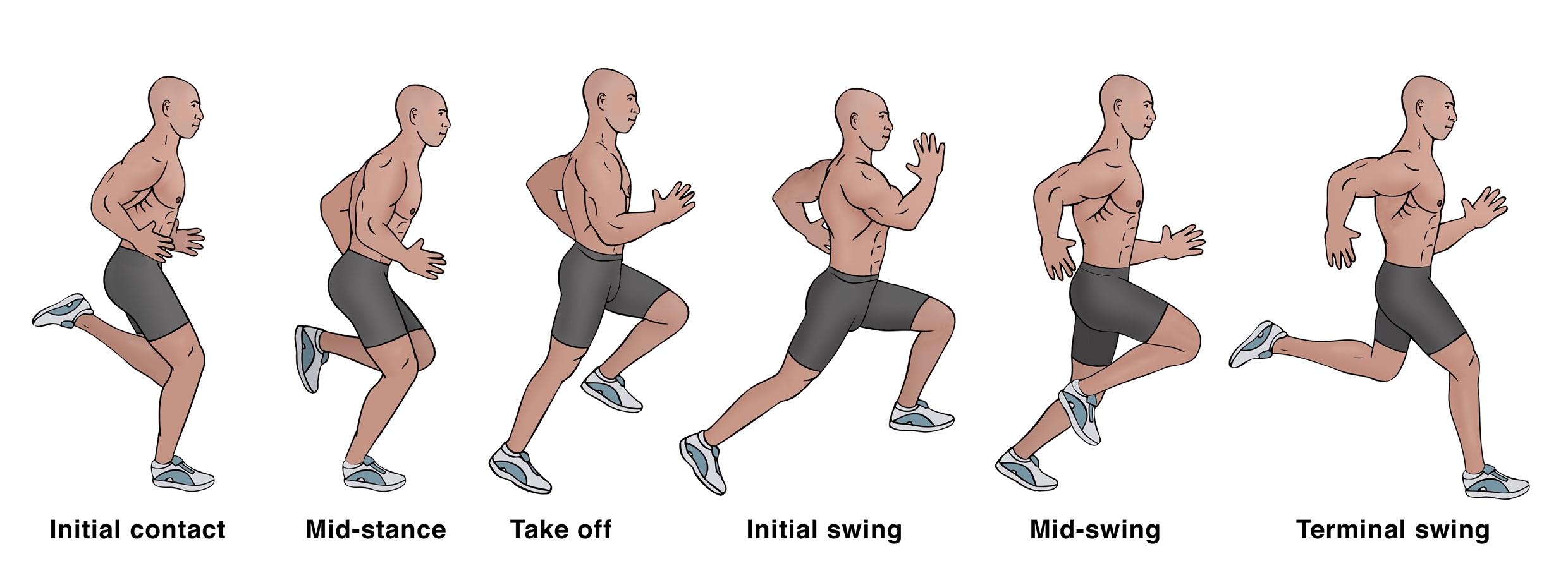
Figure 2: Biomechanics during sprinting
Table 2: British Athletics Medical Team classification
| Grading | Site (see figure 1) |
| 1 -Pain during or after activity-ROM normal at 24hr -Normal power and initiation -Pain on contraction | a-Myofascial Myofascial injury in the peripheral aspect of the muscle |
| 2 -Pain during activity and restricts participation -Limitation with ROM -Pain on contraction -Reduced power on testing | b-Musculo-tendinous Injury within the muscle belly, most commonly at musculotendon junction (MTJ) |
| 3 -Extensive tear -Sudden onset of pain -Significantly reduced ROM -Pain on walking-Obvious weakness on testing | c-Intratendinous An injury that extends into the tendon |
| 4 -Complete tear of the muscle or tendon-Sudden onset of pain-Significant limitation to activity-Palpable gap on palpitation -May be less pain than Gr3 |
Site of injury and grading classification
In a randomized controlled trial on professional Swedish footballers(1), the primary injury was located in BFLH (69%). This contrasted with 21% of the players who sustained their primary injury within SM. It was common to sustain a secondary injury to ST as well as BFLH (80%) or SM (44%). A clear majority (94%) of the primary injuries were found to be of the sprinting type and were located in the BFLH, whereas SM was the most common (76%) location for the stretching type of injury. These findings were supported in another similar article(5).
Typically, classification for acute soft tissue injury, including hamstrings, has relied on a grading system of I (mild), II (moderate), or III (severe)(see table 1)(2,6,7). This classification is useful in terms of coherent descriptions between different medical team members during clinical diagnosis and prognosis following acute injury. It has also been utilized as a classification system for radiological methods, such as magnetic resonance (MR) imaging, or ultrasound (US), if required for complementary confirmation of diagnosis(5).
The British Athletics Medical Team proposes a new injury classification system for improved diagnostic accuracy and prognostication based on MRI features (see table 2 and figure 3)(5).
Determining accurate return-to-play timescales following an acute hamstring injury has proven difficult. Injuries involving an intramuscular tendon or aponeurosis with adjacent muscle fibers (BF during high-speed running) typically require a shorter recovery period than those involving a proximal free tendon and/or MTJ (SM during dance or kicking)(2).
There are also links between MRI findings as well as the area of injury, and return-to-play. More specifically, it has been hypothesized that the shorter the distance between the proximal pole of the injury and the ischial tuberosity (i.e., more intratendinous in nature) found on MRI findings (determined by the presence of edema), the longer the time to return(1). Likewise, the length of edema shows a similar effect on recovery time – i.e., the longer the length, the longer the recovery(1). In addition, the position of peak pain upon palpation following acute injury is also linked with increased recovery periods(1).
Furthermore, there have been attempts to clarify the link between the grading of an acute hamstring injury and return to play. In a prospective cohort study on 207 professional footballers with acute hamstring injuries, 57% were grade I, 27% were grade II, and 3% were grade III. Grade I injuries returned to play within an average of 17 days. Grade II was 22 days, and grade III was 73 days. Eighty-four percent of these injuries affected the BF, 11% SM, and 5% ST, but there was no significant difference in lay-off time for injuries to the three different muscles(5). This has been compared to 5-23 days with grade I-II injuries and 28-51 days with grade I-III in other studies, respectively(1,8).
Table 1: Typical classification
| Grading | Clinical Findings |
| I (Mild) | -Small quantity of muscle fibres involved -Minor swelling Discomfort -No or only minimal loss of strength -No or only minimal restriction of movement |
| II (Moderate) | -Tear of significant number of muscle fibres -Pain and swelling -Pain reproduced on muscle contraction -Reduced power -Movement limited by pain |
| III (Severe | -Tear occurs across entire cross-section of the muscle/tendon-Commonly a tendinous avulsion -Often requires surgical opinion |
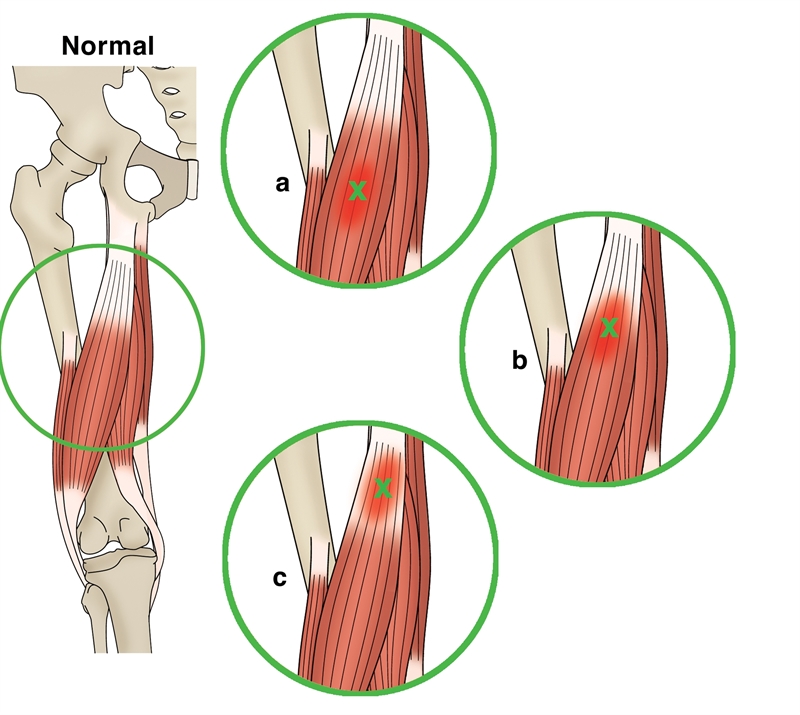
Figure 3: Letter classification dependent on anatomical site of muscle injury
Rehabilitation – eccentric strengthening
Several researchers have argued the benefits of eccentric strengthening following an acute hamstring injury versus concentric when aiming to reduce timeframes for return-to-play(1-5,9). The crux of this argument is that with the majority of acute hamstring injuries occurring during eccentric loading (terminal swing or stretching), the rehabilitation ‘should mirror the particular situation that leads to the injury’(1). This quotation was taken from a study that showed a significant difference between an eccentric and concentric rehabilitation program following acute hamstring injuries in elite and non-elite footballers.
This study was a randomized controlled clinical trial on 75 footballers in Sweden, which reported that using eccentric strengthening versus concentric, the time to return to play was reduced by 23 days. This was irrespective of the type of injury or the site of injury. The outcome measure was the number of days to return to full–team training and availability for match selection. This article will now explore this study in greater depth.
Two rehabilitation protocols were used, and initiation began five days following injury. All players had sustained a sprinting-type (high-speed running/ acceleration) or stretching-type injury (high kicking, split positions, glide tackling). Exclusion criteria included previous hamstring injuries, trauma to the posterior thigh, ongoing history of low back problems, and pregnancy.
All players underwent an MRI investigation five days following the injury to expose the severity and site of the injury. A player was judged to be fit enough to return to full-team training using the active ‘Askling H-test’ (see figure 4). A positive test is when a player experiences any insecurity or apprehension when performing the test. The test should be completed without full dorsiflexion of the ankle.


Figure 4: The Askling H-test
Seventy-two percent of players sustained sprinting-type injuries, whilst 28% were stretching-type. Of these, 69% sustained injury to BFLH, whereas 21% were located in the SM. Injuries to ST were only sustained as secondary injuries (48% with BFLH, and 44% with SM). Ninety-four percent of sprinting-type injuries were located in the BFLH, while SM was the most common (76%) location for the stretching-type injury.
The two rehabilitation protocols used were labeled L-protocol and C-protocol. One aimed at loading hamstrings during lengthening (L-protocol), and the other consisted of exercises with no emphasis on lengthening (C) (see boxes 1 and 2). Each consisted of three exercises that could be performed anywhere and were not dependent on advanced equipment. They also aimed at targeting flexibility, trunk/pelvic stability as well as specific strength training to the hamstrings. All were performed in the sagittal plane with speed and load progressed throughout.
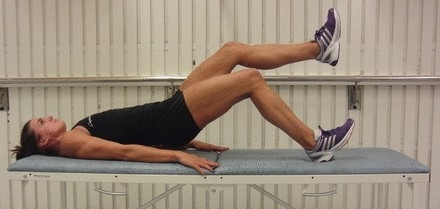
Box 1: C-Protocol
-Standing contract/relax hamstring stretch – twice every day, 3 sets x 4 repetitions.
-Standing cable/resistance band hip extension with injured limb – once every day, 3 sets x 6 repetitions.
-Supine single-leg pelvic lift using body weight on injured limb – Once every 3rd day, 3 sets with x8 repetitions.
Box 2: L-Protocol
-‘The Extender’ on injured limb (slow knee extensions to the point just before pain) – Twice daily, 3 sets x 12 repetitions.
-‘The Diver’ standing on injured limb (performed slowly with simultaneous upper and lower limb movement) – Once every other day, 3 sets x 6 repetitions.
-‘The Glider’ with injured leg in front using friction sock/ sliding matt for sliding leg (movement back to standing is completed using the arms. Progression with distance of slide and speed performed) – Once every 3rd day, 3 sets x 4 repetitions.
Findings
The time to return was significantly shorter in the L-protocol compared with the C-protocol, averaging 28 days and 51 days, respectively. Time to return was also significantly shorter in the L-protocol than in the C-protocol for injuries of both sprinting-type and stretching-type, as well as for injuries of different injury classifications. There are questions, however, over whether the C-protocol is specific enough for hamstring activation to create a legitimate comparison.
Summary and clinical implications
Acute hamstring injuries most commonly occur during sprinting (terminal swing) or stretching (kicking, sliding, lunging/split positions). BFLH is involved more often in sprinting-type injuries as a result of terminal swing. This is possibly due to its absorption of the largest peak musculotendon strain across all four hamstring muscles. Injuries can be classified from Grades I-III or, perhaps more specifically, Grades 1-4 for severity and a-c, depending on the site of injury. This is based on MRI findings. The closer the site of injury is to the proximal hamstring tendon, the longer the return-to-play period. Using eccentric strengthening exercises in rehabilitation programs will promote a faster return to play. For example, ‘The Extender’, ‘The Diver’, or ‘The Slider’. To enable a thorough rehabilitation process, clinicians need to take into account the initial hamstring weakness, any lack of flexibility, previous hamstring injuries, age, fatigue, and strength imbalances between hamstring (eccentric) and quadriceps (concentric) contraction.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.