Clearing the confusion – clinical concussion rehabilitation
Concussion research continues to gain the support of sports medicine professionals. However, many remain in the dark regarding the potential of rehabilitation to improve clinical outcomes. Megyn Robertson shines a light on vestibular and oculomotor rehabilitation following concussion. Football - Premier League - Aston Villa’s John McGinn receives medical attention before being replaced by a concussion substitute. Action Images via Reuters/Andrew Boyers
Football - Premier League - Aston Villa’s John McGinn receives medical attention before being replaced by a concussion substitute. Action Images via Reuters/Andrew Boyers
Concussion is currently one of the most intensely debated topics in sports medicine. According to the University of Pittsburgh Medical Centre (UPMC), there are between 1.7 and 3 million sports-related concussions (SRC) annually in the USA(1). In addition, the Journal of Neurosurgery states that almost 64–74 million individuals suffer from concussion cases every year(2). Concussion research is progressing, especially in incidence, assessment, and recovery. However, clinicians are still learning the most effective rehabilitation approaches for this complex injury.
What is a concussion?
A concussion is a complex pathophysiological injury affecting the brain, caused by traumatic biomechanical forces, resulting in a transient change of neurological functions caused by direct head impact or indirect blows to the body. Clinical signs and symptoms of a concussion vary hugely. They include headache, dizziness, visual disturbances, amnesia, fatigue, sleep disturbances, nausea, neck pain, balance disruptions, emotional lability, and cognitive changes such as poor memory, reaction time, and processing speed.
Post Concussion Syndrome
Eighty percent of the population who sustain a concussion will recover within 10-14 days. However, 20% have persistent symptoms, and rehabilitation can play a considerable role with early intervention. One of the rehabilitation aims is to return patients to school, work, and play in the shortest period possible. However, most importantly, the primary goal is to prevent the onset of Post Concussion Syndrome.
Some patient groups are more vulnerable to persistent concussion symptoms. For example, children and adolescents usually take longer to recover from concussions. This is primarily due to their developing brains being largely unmyelinated. In addition, their brains have a higher water content associated with incomplete neuronal synapse formation and arborization, so there is less buoyancy and, therefore, less protection than the mature brain. Furthermore, adolescents have disproportionately big heads with weak necks than adults(3). However, clinicians should expect children and teens to recover from concussions within a month without significant concerns.
Females have worse concussions and more protracted recoveries than males. Progesterone levels at the time of concussion may also play a role in delayed recoveries, dependent on the timing of their menstrual cycles. Furthermore, women have thinner axons than males, so the shear forces from a concussion are more debilitating, compounded by weaker neck strength, which also inhibits their ability to withstand greater impact forces in contact sports(4).
There is no loss of consciousness (LOC) in 90% of concussion cases. However, in situations where a LOC occurs, the longer the period of unconsciousness, the more protracted the recovery. Similarly, amnesia (anterograde or retrograde) duration is directly proportionate to the length of recovery. For example, if a patient reports dizziness at the time of injury, they are 6.3 times more likely to experience an extended recovery beyond 21 days. Furthermore, previous mood disorders such as a history of anxiety or depression are also risk factors for delayed recovery from concussion(5,6). Moreover, a history of migraines and previous significant concussions are predictors of a lengthy recovery.
There is still some controversy over whether a history of ADD/ADHD is a risk factor for prolonged recovery. Researchers at the Harvard Medical School in Boston found that ADHD is an antecedent risk factor for concussion. The researchers found that children with ADHD experience more symptoms and complications during recovery and have significantly worse deficits in executive function(7). However, on the contrary, another research group from the Harvard Medical School found that adolescents with ADHD did not take longer to functionally recover following a concussion(8). Therefore, clinicians should maintain a high degree of suspicion for prolonged recovery in children with ADHD and individualize the assessment and treatment plan to the child’s needs.
Risk factors for prolonged recover
- Child or adolescent
- Female
- Longer duration of unconsciousness or amnesia
- Dizziness at time of injury
- Mood disorders
- Migraine history
- Concussion history
Balancing act: the postural control system
Postural control is how our central nervous system (CNS) regulates sensory information to produce adequate motor output to maintain a controlled, upright posture against gravity. The integration of visual, vestibular, and somatosensory components maintains postural balance. The postural control system is affected by a concussion, and therefore, the assessment and treatment of a concussion require a multifaceted approach.
The Visual System
A diffuse brain injury will often affect the visual system as more than half of the brain’s pathways control vision and eye movements(9). In addition, visual disorders may occur in up to 69% of patients following mild traumatic brain injuries (mTBI), with accommodative and convergence insufficiencies being the most prevalent in the general population(10). Vision problems that develop after a concussion are not acuity-related; instead, they are eye teaming, focusing, and tracking, creating difficulties with reading and sports. This may be due to the widespread neural architecture of the visual system, which includes frontal and posterior cortical regions, cerebellum, cranial nerves, and interconnections between these areas. The neurometabolic and structural impacts of concussion in the form of diffuse axonal injury render the visual brain especially vulnerable. Therefore, oculomotor dysfunction is common, and patients may present with headaches, blurred vision, double vision, eye strain, and functional difficulty with activities such as reading and computer work(11).
What is BPPV?
Benign paroxysmal positional vertigo is the most common form of vertigo that occurs with positional head changes.
Clinicians can treat BPPV using the(canalith repositioning maneuver). The goal is to move the Otoconia (CaCO3 crystals) from the semicircular canals back into the otolithic organs in the ear.
Vestibular Oculomotor Screening (VOMS)
A valid and reliable screening tool exists to assess the vestibular and oculomotor systems following concussion(12). The assessment tool, knowns as VOMS, detects concussion signs and symptoms and is accurate when combined with a clinical interview, symptom assessment, and computerized neurocognitive testing, e.g., Cogstate or Impact. The VOMS assesses the systems responsible for integrating balance, vision, and movement. Furthermore, it requires little equipment (a tape measure and a metronome) and takes under 10 minutes to complete (see table 1)(12).
Table 1: Vestibular Oculomotor Screening (VOMS)(12).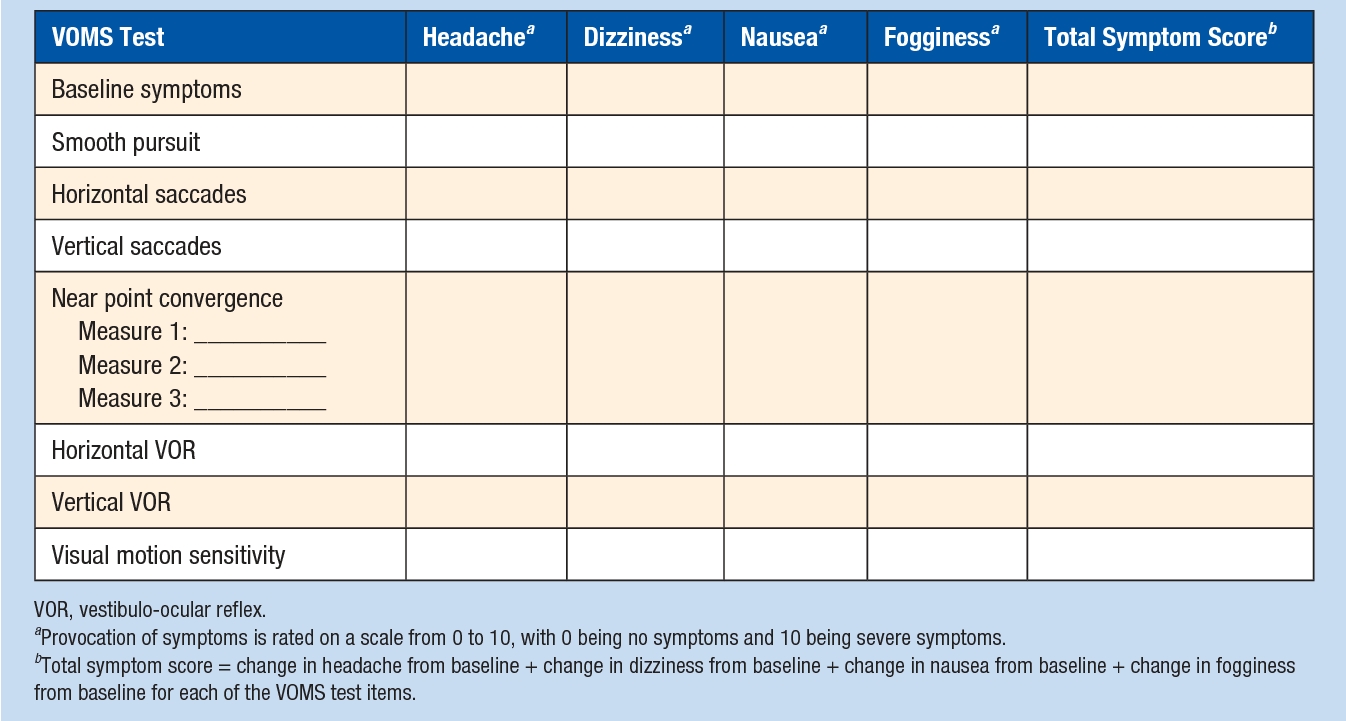
Concussion rehabilitation
Vision therapy is an effective treatment modality for concussions(13). Vestibular therapy effectively manages dizziness, imbalance, and spatial orientation. Neurocognitive and neuromotor changes after a concussion may affect injury risk. In addition, a history of concussion impairs athletic performance through impaired dynamic stability and obstacle avoidance, suggestive of deficits in executive functioning, spatial awareness, and rapid information processing that may contribute to subsequent lower extremity (LE) injury risk. The risk for LE injury is 45% greater in those with a concussion, and the risk remains elevated for more than a year following injury(15).
It is essential that clinicians screen for vestibular and oculomotor dysfunction after a concussion. The initiation of an active, expose-recover rehabilitation approach may reduce impairments and symptoms within a month of injury(14). However, clinicians should individualize concussion rehabilitation as no single rehabilitation strategy is effective for all patients recovering from a concussion, requiring personalized treatment(16).
In conclusion, as concussion research continues to evolve, clinicians are provided with multiple options to support patients post-concussion. However, there is a need for more high-level evidence to improve the effectiveness of screening tools and rehabilitation strategies for both vestibular and oculomotor impairments post-concussion. Although concussion remains a challenge within sports and exercise medicine, clinicians do have opportunities to provide patients with proactive treatment options.
References
- University of Pittsburgh Medical Center (UPMC). Concussion facts and statistics. 2019.
- J Neurosurg. 2018;130:(4)1080-1097.
- Cantu and Hyman. Concussions and Our Kids. Mariner Books 2013.
- 2007;61(6):1244-1253.
- Handb Clin Neurol. 2018;158:163-178.
- J Neurosurg Pediatr. 2015;15(6):589-98.
- Neurol Clin Pract. 2018; 8(5): 403–411.
- Front Pediatr. 2021; 8: article 606879.
- Handb Clin Neurol. 2018;158:145–52.
- Clin Pediatr (Phila). 2016;55(3):260–67.
- Clin Neurol. 2018;158:135-144.
- Sports Health. 2017;9(2):174-180.
- Optom Vis Sci. 2016;93:00-00.
- J Athl Train. 2017;52(3):256-261.
- 2018;48(7):533–540.
- J ESSKA. 2014;22(2):235–46.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










