Sure footing: why the foot is the foundation of sports rehabilitation

The foot and ankle complex controls balance and posture and counteracts gravitational forces. The body’s natural sway posture is a flexion-based movement. Therefore, the body uses extension to counteract this. This optimal lever comes solely from the ankle joint, where isometric plantarflexion forces offset forward postural sway(1).
When the foot initially contacts the ground and moves through the mid-stance phase where the foot is flat, the foot and ankle absorb 0.8-1.2 times body weight(2). As the foot moves through mid-stance and controls dorsiflexion, this load reduces slightly and increases to more than body weight as the heel lifts in to toe-off. Therefore, in one gait cycle, there are two periods of force absorption greater than body weight. This repetitious cycle means extensive loading occurs each day through the foot and ankle during activities of daily living.
Progression to running increases the load through the tibia to two times body weight, and the tibia will experience bone stress at loads greater than this(3). Excessive loading results in conditions such as medial tibial stress syndrome, plantar fasciitis, and achillodynia. These loads are primarily counteracted by the soleus muscle, which can absorb up to six times body weight(3).
With a progression to elite-level sprinting, the foot and ankle will absorb up to 12.5 times body weight within a short timeframe and require the Achilles tendon and calf muscles to counteract these forces(4). This increased absorption via the gastrocnemius and soleus muscles reduces the demand on the anterior hip joint and musculature to bring the hip forwards. Ensuring optimal calf strength minimizes the risk of groin and hip flexor injures.
Withstanding the large forces exhibited upon the foot and ankle requires a synergy between the lower limb muscles and the architecture and biomechanics of the foot. Failure of any part of this mechanism will result in overload and injury. Therefore, it is imperative to treat the foot and ankle as components of the entire lower body kinetic chain rather than isolated joints or structures. For example, don’t just treat a gastrocnemius strain with gastrocnemius strengthening exercises. Instead, consider the surrounding articular and muscular systems and the end goal of the athlete to ensure they are fit for their sport.
Foot and ankle functions
The foot and ankle complex is responsible for a diverse range of functions, from static posture to complex dynamic activity. It provides:- In standing - a base of support and counteracts gravity for balance;
- In gait - stability at foot-strike and push off for propulsion and efficient muscle force;
- In mid-support - flexibility to accommodate terrain and attenuate load;
- Shock absorption - through the three rocker system;
- Spring-like characteristics which store, conserve, and release elastic energy with each foot strike(2,5).
Failure of any of these functions results in an unstable foundation, malalignment, and possible pathologies, such as plantar fasciitis, posterior tibial tendon dysfunction, and medial tibial stress syndrome(5). Compromise of this system may also cause the development of a secondary pathology due to compensatory movements higher up the kinetic chain, like low back pain and knee and hip injuries.
Lower limb and foot morphology
The foot and ankle complex is comprised of 25 small bones, 33 joints, and over 100 muscles, tendons, and ligaments that all coordinate for optimal movement. Sometimes, structural morphology is inflexible. Therefore, it is imperative to understand the morphology and influence muscle strength to support the architecture. Genu valgus (knees inward) causes early foot pronation and increased activation of the lateral musculature. In contrast, genu varum (knees outward) results in late foot pronation and increased demand on the medial musculature.It is also important to evaluate the foot’s structure. A pes cavus foot has a high longitudinal arch which can be rigid or mobile. A rigid foot is sagittal plane dominant and lacks the mobility to move throughout the gait cycle. A mobile foot is coronal/rotational plane dominant and has so much flexibility it may lack adequate stability. Pes equinus is a rigid cavus foot that cannot dorsiflex as the talus abuts against the tibia. This limitation creates excessive midfoot overload. Pes planus is a loss of the medial longitudinal arch (flat foot dysfunction) and increases the demand on the arches.
Rockers and arches
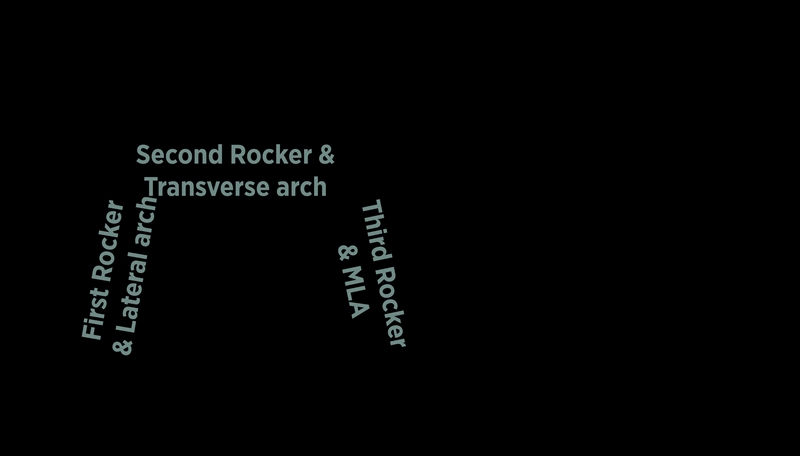
Three rockers coordinate the flow from heel strike to toe-off throughout the gait cycle. Rockers control motion, help with efficient movement of loads greater than body weight, and store elastic energy to dissipate forces during the gait cycle.Figure 1: The gait cycle detailing the three foot rockers.

The first rocker occurs from heel strike to foot flat. The foot may fall into early pronation without adequate control here, which can overload the subtalar joint, spring ligament, and tibialis posterior and compress the big toe. The second rocker arises in mid-stance when the foot is flat, and the tibia moves over the talus, creating 10 to 20 degrees of dorsiflexion. Without proper ankle mobility, compensations occur through rotational patterns. The third rocker happens when rolling through mid-stance to heel lift and toe-off. This rocker stores and releases energy to enhance gait efficiency. Dysfunction here reduces energy transfer and overloads the big toe and the arches.
The arches create tensegrity, a system of tension around the articular structures, which fosters stability and is crucial in regulating the complexity of the foot joints(6). The three arches are the lateral longitudinal arch, medial longitudinal arch (MLA), and transverse arch. As the foot moves through the first rocker at heel strike, the lateral arch absorbs the load. The load then transfers to the transverse arch as the second rocker operates through mid-stance, and then the medial longitudinal arch absorbs the load as the foot moves into pronation and the third rocker mechanism. One arch cannot work effectively if another is dysfunctional. Their function relies on the transference of elastic energy through the biomechanical mechanisms(2). During dysfunction, compensations like tibial rotation and hip adduction occur and strain the surrounding soft tissues.
Figure 2: A graph detailing gait forces and the role of the rockers and arches.
The foot core system
The arches of the foot function similarly to the core stabilizers within the trunk. The intrinsic foot muscles act as the deep local stabilizers that control the arches, and the lower limb muscles are the global movers that allow locomotion(5). To assess foot core function, perform the ‘intrinsic foot muscle test’(7). Ask the athlete to maintain a neutral foot posture and MLA height while balancing on one leg for 30 seconds (foot core). Note any compensations, including their origin from higher up the limb. To train the foot core, perform the ‘short foot exercise’ to isolate the intrinsic muscles (see figure 3)(8). This exercise develops muscle control similar to the core engagement exercise used in trunk core activation. Ask the athlete to shorten their foot length using the intrinsic muscles, pulling the big toe towards the heel, and elevating the MLA to create a dome shape. Perform the short foot exercise for four weeks to reduce arch collapse, improve balance and great toe strength, and decrease ankle instability(9, 10, 11, 12).Figure 3: The short foot exercise.

The top image shows the relaxed foot position and starting position for the short foot muscle exercise. The second image shows the shortening of the plantar aspect and a doming of the arch(8).
Coordinating the correct exercise and prescription to target the goal is key to successful rehabilitation. Include the foot and ankle complex as part of the core rehabilitation for most lower limb injuries(2).
| Exercise | Description | Prescription | Benefits |
|---|---|---|---|
| Single leg calf raises | Performed on a step without letting the heel drop below the step. | 3 x 15. Repeat 4 times to total 180 repetitions per ankle. | Completed to failure to ensure endurance. |
| High repetitions and tempo to allow transfer of energy to non-contractile tissue. | |||
| Isometric calf raises | Long holds for pain modulation >45 sec. | Elite: 3 xBW for 5 repetitions. 4-8 sets. | Target both gastrocnemius and soleus. |
| Provides inner range hold. | |||
| Short holds for force production < 6s. | Amateur: BW x5 repetitions. 3-4 sets. | Loads plantar fascia, small foot muscles, and equally loads metatarsal heads. | |
| Plie calf raises | Calf raises with feet turned out, heels together, knees slightly flexed. | 4x25. | Inner range load. |
| Elite: Males BW on barbell. | Bias to tendon and non-contractile tissue. | ||
| Females 50% BW on barbell. | Modifiable for eccentric control. | ||
| Amateur: BW. | |||
| Seated calf raises | Squat position and lean back holding on to a Smith machine. | Elite: 40-60kg+ 4x30. 2 minutes per set. | Soleus bias. |
| Inner range loading. | |||
| Single leg raises with kettlebell on knee. | Deep medial and lateral compartments also loaded. | ||
| Amateur: BW for 3x30. 2 minutes per set. | |||
| Tibialis anterior bias | Seated dorsiflexion with weight disc on foot. | 10kg weight for 4x30. | Biomechanical advantage in knee flexion. |
| Synergy with other anterior muscles. | |||
| Stiffness through non-contractile tissue. | |||
| Cocky walks | Walking on tiptoes with feet externally rotated and a weight above the head. | Functional. | |
| Adds hip control. | |||
| Includes postural challenge with added load. | |||
| Centre of mass and base of support challenge. |
Exercise prescription considerations
To ensure specificity in exercise prescription and induce hypertrophy in targeted regions, consider the following:1) Foot position
Altering the foot position can influence bias towards specific muscles and obtain selective muscle hypertrophy. Performing calf raise style exercises with the foot pointing inwards will bias the lateral gastrocnemius head, and with the foot pointing outwards will produce medial head hypertrophy(13). Positioning the foot forwards results in a similar growth in both gastrocnemius heads(13).
2) Knee position
Performing the exercises with the knee flexed to approximately 30 degrees or more will bias the soleus. As the soleus supports up to six times body weight, this is crucial to include in any program, even if it is not the primary target(3). Seated calf raises are a common choice for knee flexion-based calf raises. However, as these are non-weight bearing, add enough weight to the knees to ensure adequate loading(14).
3) Weight-bearing or non- weight bearing
Seated calf raises and those done on the leg press machine allow optimal positioning and addition of load. However, they lack weight-bearing functionality. Performing wall squats with heels raised will tackle both elements and allow flexibility with double or single leg options.
Summary
The foot and ankle complex is responsible for a diverse range of functions that rely on the intricate coordination of many joints and muscles. The rockers and the arches must function in harmony for optimal locomotion. The foot must be well adapted to absorb tremendous forces as the athlete shifts from walking to running and sprinting. Dysfunction anywhere within this architecture can cause overload to the lower back, hips and legs. Maintaining adequate strength in the foot and ankle muscles can help prevent injuries elsewhere.References
- J Am Podiatr Med Assoc.1999; 89(3): 109–117.
- www.hd-pn.com/. Sporting Foot & Ankle.
- J of Biomechan. 2007; 40: 3503–3509.
- . Europ J of Appl Physiol and Occ Physiol. 1980; 44:279-289.
- Br J Sports Med. 2015; 49:290. Doi:10.1136/bjsports-2013-092690.
- Rep Prog Phys. 2014; 77(4): 046603. doi:10.1088/0034-4885/77/4/046603.
- www.aptei. com/articles/pdf/IntrinsicMuscles.pdf. 2013.
- Liebenson C. ed Rehabilitation of the Spine: a practitioner’s manual. 2nd ed.
- Lippincott Williams & Wilkins, 2006.
- Man Ther. 2013; 18:425–30.
- J Sport Rehabil. 2012;21:327–33.
- J Back Musculoskelet Rehabil. 2011;24:225–31.
- J Athl Train. 2010;45:S67.
- J Strength Cond Res. 2020; 34(8): 2347- 2351.
- Am J Sports Med. 2015; 43(7): 1704-1711.
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










